Bibliographie de Médecine d'Urgence
Academic Emergency Medicine
Central nystagmus plus ABCD2 identifying stroke in acute dizziness presentations.
Wang W, Zhang Y, Pan Q, Liu J, Zhu Y, Tan G, Zhan Q, Zhou J. | Acad Emerg Med. 2021 Oct;28(10):1118-1123
DOI: https://doi.org/10.1111/acem.14295
Keywords: ABCD2 scores; HINTS; acute dizziness; nystagmus; stroke.
ORIGINAL CONTRIBUTIONS
Introduction : The objective was to explore the ability of head impulse-nystagmus-test of skew (HINTS) combined with ABCD2 score to identify cerebrovascular causes of dizziness.
Méthode : We prospectively recruited 85 patients with acute onset of dizziness from September 2016 to December 2018 and analyzed their clinical characteristics, ABCD2 scores, HINTS, and neuroimages data.
Résultats : Acute stroke was identified by MRI in 21 of 85 patients. The mean ± SD ABCD2 scores were significantly higher among patients with acute stroke than those without acute stroke (4.0 ± 0.8 h vs. 2.5 ± 0.7 h, p < 0.01). The majority (71.4%) of patients with cerebrovascular causes had central pattern of nystagmus at the initial 48 h from symptoms onset. The sensitivity and specificity of HINTS were 100% and 87% for the presence of stroke in patients with nystagmus. When combined central pattern of nystagmus and ABCD2 ≥ 4, the sensitivity increased to 100% for identifying cerebrovascular causes. Nystagmus were absence at time of examination in 16.5% of our patients, and ABCD2 scores in patients who had cerebrovascular diagnoses were all ≥ 4.
Conclusion : HINTS examinations could efficiently differentiate stroke from nonstroke under the condition that patients remaining symptomatic, including spontaneous or gaze-evoked nystagmus. It is more practical to apply the combination of central pattern of nystagmus and ABCD2 ≥ 4 in ED setting. If patients were absence of central nystagmus at admission, cerebrovascular event should be a priority diagnosis when their ABCD2 ≥ 4.
Conclusion (proposition de traduction) : La séquence de tests cliniques HINTS pourrait différencier efficacement les accidents vasculaires cérébraux des non-AVC à condition que les patients restent symptomatiques, y compris avec un nystagmus spontané ou provoqué par le regard. Il est plus pratique d'appliquer la combinaison de l'origine centrale du nystagmus et le score ABCD2 ≥ 4 dans le cadre d'un service d'émergence. Si les patients ne présentaient pas de nystagmus central à l'admission, un accident vasculaire cérébral devrait être recherché en priorité lorsque leur score ABCD2 est ≥ 4.
Commentaire : Le HINTS est une séquence de tests cliniques permettant de dissocier les origines périphériques des causes centrales. Dans un syndrome vestibulaire isolé, le « HINTS » est même plus sensible en phase aiguë que l’IRM pour le diagnostic d’un AVC.
La batterie de tests du HINTS est simple et fiable. Elle permet de diagnostiquer avec une sensibilité et une spécificité toutes deux supérieures à 80 % l’origine centrale d’un vertige aigu.
La présence simultanée d’un nystagmus de type central, d’un HIT normal et d’un Cover Test positif signifie que le patient présente en première hypothèse une pathologie centrale aiguë à prendre en charge en urgence en unité neuro-vasculaire.
Peschanski N. Vertiges aux urgences – Y’a comme un hic dans le HINTS ! . Septembre 2021.
Kattah JC, Talkad AV, Wang DZ, Hsieh YH, Newman-Toker DE. HINTS to diagnose stroke in the acute vestibular syndrome: three-step bedside oculomotor examination more sensitive than early MRI diffusion-weighted imaging. Stroke. 2009 Nov;40(11):3504-10

L’accident ischémique transitoire (AIT) est suivi chez 10 à 20 % des patients d’un AVC dans les trois mois, et représente donc une urgence relative de prise en charge. Le score ABCD2 (A = Age, B = Blood pressure hypertension, C = déficit Clinique D = Diabète, D = Durée) est bien validé pour prédire le risque immédiat et tardif d’AVC.
Le score ABCD2 permet de catégoriser trois groupes de risque ; bas : < 4 points, modéré : 4-5 points, ou élevé : > 5 points).
Toutefois, le score ABCD2 stratifie correctement le risque, en le surestimant. Mais une stratégie de prise en charge basée sur son utilisation ne s’accompagne pourtant pas d’une augmentation du risque d’AVC.
PECARN algorithms for minor head trauma: Risk stratification estimates from a prospective PREDICT cohort study.
Bressan S, Eapen N, Phillips N, Gilhotra Y, Kochar A, Dalton S, Cheek JA, Furyk J, Neutze J, Williams A, Hearps S, Donath S, Oakley E, Singh S, Dalziel SR, Borland ML, Babl FE; Paediatric Research in Emergency Departments International Collaborative (PREDICT). | Acad Emerg Med. 2021 Oct;28(10):1124-1133
DOI: https://doi.org/10.1111/acem.14308
Keywords: PECARN; child; clinical decision rule; traumatic brain injury.
ORIGINAL CONTRIBUTIONS
Introduction : The Pediatric Emergency Care Applied Research Network (PECARN) head trauma clinical decision rules informed the development of algorithms that risk stratify the management of children based on their risk of clinically important traumatic brain injury (ciTBI). We aimed to determine the rate of ciTBI for each PECARN algorithm risk group in an external cohort of patients and that of ciTBI associated with different combinations of high- or intermediate-risk predictors.
Méthode : This study was a secondary analysis of a large multicenter prospective data set, including patients with Glasgow Coma Scale scores of 14 or 15 conducted in Australia and New Zealand. We calculated ciTBI rates with 95% confidence intervals (CIs) for each PECARN risk category and combinations of related predictor variables.
Résultats : Of the 15,163 included children, 4,011 (25.5%) were aged <2 years. The frequency of ciTBI was 8.5% (95% CI = 6.0%-11.6%), 0.2% (95% CI = 0.0%-0.6%), and 0.0% (95% CI = 0.0%-0.2%) in the high-, intermediate-, and very-low-risk groups, respectively, for children <2 years and 5.7% (95% CI = 4.4%-7.2%), 0.7% (95% CI = 0.5%-1.0%), and 0.0% (95% CI = 0.0%-0.1%) in older children. The isolated high-risk predictor with the highest risk of ciTBI was "signs of palpable skull fracture" for younger children (11.4%, 95% CI = 5.3%-20.5%) and "signs of basilar skull fracture" in children ≥2 years (11.1%, 95% CI = 3.7%-24.1%). For older children in the intermediate-risk category, the presence of all four predictors had the highest risk of ciTBI (25.0%, 95% CI = 0.6%-80.6%) followed by the combination of "severe mechanism of injury" and "severe headache" (7.7%, 95% CI = 0.2%-36.0%). The very few children <2 years at intermediate risk with ciTBI precluded further analysis.
Conclusion : The risk estimates of ciTBI for each of the PECARN algorithms risk group were consistent with the original PECARN study. The risk estimates of ciTBI within the high- and intermediate-risk predictors will help further refine clinical judgment and decision making on neuroimaging.
Conclusion (proposition de traduction) : Les estimations du risque de lésion cérébrale traumatique cliniquement importante pour chacun des groupes de risque des algorithmes PECARN étaient cohérentes avec l'étude PECARN originale. Les estimations du risque de lésion cérébrale traumatique cliniquement importante dans les prédicteurs de risque élevé et intermédiaire aideront à affiner davantage le jugement clinique et la prise de décision de neuroimagerie.
Commentaire : Le traumatisme crânien léger de l’enfant est un motif fréquent de recours aux services d’urgence. Il est défini par un score de Glasgow ≥ 13 et représente plus de 95 % des traumatismes crâniens. Parmi les enfants présentant un traumatisme crânien léger, moins de 10 % ont une lésion intracrânienne et moins de 1 % ont besoin d’une intervention neurochirurgicale.
Le Pediatric Emergency Care Applied Research Network (PECARN) est utilisé dans la prise en charge du TCL de l’enfant pour identifier parmi ces enfants peu symptomatiques ceux à risque de lésion intracrânienne qui nécessiteront un scanner cérébral rapide afin de ne pas exposer inutilement des enfants à des radiations ionisantes potentiellement iatrogènes. Cette règle de décision clinique permet de classer l’enfant, à partir d’éléments de l’interrogatoire et de l’examen clinique, en trois niveaux de risque de lésion intracrânienne cliniquement sévère : haut, intermédiaire ou faible ; et ainsi d’orienter sa prise en charge : scanner cérébral, surveillance hospitalière ou retour à domicile (Société française de médecine d’urgence et reprises par le Groupe francophone de réanimation et urgences pédiatriques).
 Lorton F, Vrignaud B, Gras-Le Guen C. Traumatisme crânien léger de l'enfant . Pas à pas en pédiatrie, Arbres décisionnels commentés des sociétés de pédiatrie. Août 2019.
Lorton F, Vrignaud B, Gras-Le Guen C. Traumatisme crânien léger de l'enfant . Pas à pas en pédiatrie, Arbres décisionnels commentés des sociétés de pédiatrie. Août 2019.
• Recommandations du GFRUP sur la prise en charge du traumatisme crânien léger de l'enfant (2014)
• Plaquette d'information à destination des enfants et faite par France Traumatisme Crânien.
Kuppermann N and al. Identification of children at very low risk of clinically-important brain injuries after head trauma: a prospective cohort study. Lancet. 2009 Oct 3;374(9696):1160-70 .
The association of ketamine induction with blood pressure changes in paramedic rapid sequence intubation of out-of-hospital traumatic brain injury.
Fouche PF, Meadley B, St Clair T, Winnall A, Jennings PA, Bernard S, Smith K. | Acad Emerg Med. 2021 Oct;28(10):1134-1141
DOI: https://doi.org/10.1111/acem.14256
Keywords: blood pressure; interrupted time series; paramedic; quazi-experiment; rapid sequence intubation; traumatic brain injury.
ORIGINAL CONTRIBUTION
Introduction : Rapid sequence intubation (RSI) is used to secure the airway of traumatic brain injury (TBI) patients, with ketamine frequently used for induction. Studies show that ketamine-induction RSI might cause lower blood pressures when compared to etomidate. It is not clear if the results from that research can be extrapolated to systems that use different dosing regimens for ketamine RSI. Ambulance Victoria authorized the use of 1.5 mg/kg ketamine in January 2015 for head injury RSI induction by road-based paramedics. This study aims to examine whether systolic blood pressure changed when ketamine was introduced for prehospital head injury RSI.
Méthode : This study was a retrospective analysis of out-of-hospital suspected TBI that received RSI by paramedics. Our analysis employs an interrupted time-series analysis (ITSA), which is a quasi-experimental method that tested whether hypotension and systolic blood pressures changed after the switch to ketamine induction in 2015. This ITSA utilized an ordinary least squares regression on complete observations using Newey-West standard errors.
Résultats : During the study period, paramedics performed RSI in 8,613 patients, and 1,759 (20.4%) had a TBI. Ketamine usage increased by 52.7% in January 2015 (p < 0.001) after road-based paramedics were authorized to use ketamine induction. This analysis found significant 5% increase in post-RSI hypotension (p = 0.046) after the introduction of ketamine, and thereafter the incidence of post-RSI hypotension increased steadily by 0.5% every 3 months (p = 0.004). Concurrently, changes in systolic blood pressure, as measured by the interval just before induction to the last measured on scene, show an average decrease of 7.8 mm Hg (p = 0.04) at the start of 2015 with the ketamine rollout.
Conclusion : This ITSA shows that postinduction hypotension and also decreases in systolic blood pressures became evident after the introduction of ketamine. Further research to investigate the association between ketamine induction and survival is needed.
Conclusion (proposition de traduction) : Cette étude de série chronologique interrompue montre qu'une hypotension post-induction et des diminutions de la pression artérielle systolique sont apparues après l’introduction de la kétamine. D’autres recherches sont nécessaires pour étudier l’association entre l’induction de la kétamine et la survie.
Commentaire : Voir une analyse de l'article sur :
Hypotension dans l’induction séquence rapide
Second (et dernier ?) crash-test pour la kétamine ! .
Une série temporelle, ou série chronologique, est une suite de mesures qui représentent un évolution de quelque chose au cours du temps.
Pour chercher à contrôler l’effet d’autres événements possibles (traitements…) sur un groupe expérimental donné, on utilise la série chronologique interrompue pour laquelle les données sont recueillies à différents moments, avant, durant et après la mise en oeuvre de la nouvelle pratique et voir si des changements significatifs pourraient être attribuables à la nouvelle pratique mise en oeuvre.
C'est donc une étude où l’on fait des observations à différents moments avant et après une intervention. Les mesures sont interrompues par l’intervention. Cette méthode vise à déterminer si une intervention donnée a eu un effet significativement plus important que toute tendance sous-jacente au fil du temps.
• Forces : Peut être réalisable et relativement facile à mener si l’on dispose des données nécessaires. Aucun groupe témoin requis.
• Faiblesses : L’ampleur de l’effet est toujours difficile à estimer dans ce genre d’analyses parce que des influences autres que l’intervention à l’étude peuvent influer sur les changements observés.
Hot off the press: the RAMPED trial-methoxyflurane for analgesia in the emergency department.
Bond C, Westafer L, Challen K, Milne WK. | Acad Emerg Med. 2021 Oct;28(10):1179-1182
DOI: https://doi.org/10.1111/acem.14257
Keywords: Aucun
Hot off the press
Editorial : Pain is one of the primary reasons that patients present to the emergency department (ED). Oligoanalgesia is a significant problem and effective pain management is an important indicator of the quality of patient care. Multiple factors have been thought to contribute to oligoanalgesia including overcrowding, language barriers, age, sex, ethnicity, and insurance status. Delays in providing adequate analgesia lead to poorer patient outcomes, prolonged ED length of stay, and reduced patient satisfaction. Previous research in Australian EDs has shown that the median time to analgesia administration can be between 40 and 70 minutes, while one study in the United States reported a mean of 116 minutes. To minimize delays, various strategies have been implemented to address the problem, including the use of novel analgesic agents that do not require intravenous access. Recently, there has been increased interest in using methoxyflurane (Penthrox), an inhaled nonopioid volatile anesthetic, to provide rapid shortterm analgesia. In Australia, methoxyflurane has been widely used at subanesthetic doses for analgesia in the prehospital setting since 1975. It has been used more widely recently and at low doses and has a very reassuring safety profile, with no reports of addiction or abuse related to its use. The majority of studies of methoxyflurane for pain focus on traumatic pain; this study aimed to assess its effectiveness in treatment of both traumatic and nontraumatic pain.
Conclusion : This is a randomized controlled trial of adult ED patients with severe pain, defined by an initial numeric rating scale (NRS) pain score of greater than or equal to 8 on an 11-point scale. Treatment arm participants were given inhaled methoxyflurane at ED triage and the comparison group received standard analgesic care, which could include acetaminophen, nonsteroidal antiinflammatory drugs (NSAIDs), tramadol, oral oxycodone, or intravenous morphine. The primary outcome was the proportion of patients who had at least a 50% reduction in pain score at 30 minutes. Secondary outcomes included median pain score at 15, 30, 60, and 90 minutes; the proportion of patients that achieved a >2-point drop in their NRS pain score, and data pertaining to adverse effects.
Conclusion (proposition de traduction) : Il s'agit d'un essai contrôlé randomisé portant sur des patients adultes souffrant de douleur sévère aux urgences, définie par un score initial de douleur sur une échelle d'évaluation numérique supérieur ou égal à 8 sur une échelle de 11 points. Les participants du groupe de traitement ont reçu du méthoxyflurane inhalé lors du triage à l'arrivée aux urgences et le groupe de comparaison a reçu des soins analgésiques standard, qui pouvaient inclure de le paracétamol, un anti-inflammatoires non stéroïdiens (AINS), du tramadol, de l'oxycodone orale ou de la morphine intraveineuse. Le critère de jugement principal était la proportion de patients qui présentaient une réduction d'au moins 50 % du score de douleur à 30 minutes. Les critères de jugement secondaires comprenaient le score de douleur médian à 15, 30, 60 et 90 minutes ; la proportion de patients ayant obtenu une baisse de > 2 points de leur score de douleur sur une échelle d'évaluation numérique et les données relatives aux effets indésirables.
Commentaire : Ricard-Hibon A et al. Inhaled methoxyflurane for the management of trauma related pain in patients admitted to hospital emergency departments: a randomised, double-blind placebo-controlled trial (PenASAP study). Eur J Emerg Med. 2020;414–21 .
American Journal of Respiratory and Critical Care Medicine
The Effect of Epinephrine Dosing Intervals on Outcomes from Pediatric In-Hospital Cardiac Arrest.
Kienzle MF, Morgan RW, Faerber JA, Graham K, Katcoff H, Landis WP, Topjian AA, Kilbaugh TJ, Nadkarni VM, Berg RA, Sutton RM. | Am J Respir Crit Care Med. 2021 Oct 15;204(8):977-985
DOI: https://doi.org/10.1164/rccm.202012-4437oc
Keywords: child; epinephrine; heart arrest.
Pediatric Critical Care
Introduction : Animal studies of cardiac arrest suggest that shorter epinephrine dosing intervals than currently recommended (every 3-5 min) may be beneficial in select circumstances.
Objectives: To evaluate the association between epinephrine dosing intervals and pediatric cardiac arrest outcomes.
Méthode : Single-center retrospective cohort study of children (<18 years of age) who received ⩾1 minute of cardiopulmonary resuscitation and ⩾2 doses of epinephrine for an index in-hospital cardiac arrest. Exposure was epinephrine dosing interval ⩽2 minutes (frequent epinephrine) versus >2 minutes. The primary outcome was survival to hospital discharge with a favorable neurobehavioral outcome (Pediatric Cerebral Performance Category score 1-2 or unchanged). Logistic regression evaluated the association between dosing interval and outcomes; additional analyses explored duration of cardiopulmonary resuscitation (CPR) as a mediator. In a subgroup, the effect of dosing interval on diastolic blood pressure was investigated.
Résultats : Between January 2011 and December 2018, 125 patients met inclusion/exclusion criteria; 33 (26%) received frequent epinephrine. Frequent epinephrine was associated with increased odds of survival with favorable neurobehavioral outcome (adjusted odds ratio, 2.56; 95% confidence interval, 1.07-6.14; P = 0.036), with 66% of the association mediated by CPR duration. Delta diastolic blood pressure was greater after the second dose of epinephrine among patients who received frequent epinephrine (median [interquartile range], 6.3 [4.1 to 16.9] vs. 0.13 [-2.3 to 1.9] mm Hg; P = 0.034).
Conclusion : In patients who received at least two doses of epinephrine, dosing intervals ⩽2 minutes were associated with improved neurobehavioral outcomes compared with dosing intervals >2 minutes. Mediation analysis suggests that improved outcomes are largely due to frequent epinephrine shortening duration of CPR.
Conclusion (proposition de traduction) : Chez les patients ayant reçu au moins deux doses d'adrénaline, des intervalles de dosage ⩽ à 2 minutes ont été associés à des résultats cognitifs améliorés par rapport à des intervalles de dosage > à 2 minutes. L'analyse de médiation causale suggère que l'amélioration des résultats est en grande partie attribuable à la fréquence d'administration de l'adrénaline qui raccourci la durée de la RCP.
Commentaire :  La figure illustre l'analyse visant à évaluer si, l'association entre la fréquence d'administration d'adrénaline et le retour à une circulation spontanée, dépendait du temps. La ligne pointillée représente le groupe administration adrénaline fréquente ; la ligne continue représente le groupe administration d'adrénaline non fréquente.
La figure illustre l'analyse visant à évaluer si, l'association entre la fréquence d'administration d'adrénaline et le retour à une circulation spontanée, dépendait du temps. La ligne pointillée représente le groupe administration adrénaline fréquente ; la ligne continue représente le groupe administration d'adrénaline non fréquente.
CPR = cardiopulmonary resuscitation (réanimation cardio-pulmonaire).
L'analyse de médiation causale est une méthode statistique permettant d'étudier les mécanismes définissant les relations entre trois entités, la première étant une cause, la deuxième une variable de réponse et la troisième un ensemble de variables intermédiaires, aussi appelés médiateurs.
1. Baron, R.M. and D.A. Kenny, The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology , 1986. 51(6): p. 1173-82.
2. Sobel, M.E., Asymptotic confidence intervals for indirect effects in structural equations models, in Sociological methodology 1982, S. Leinhart, Editor. 1982, Jossey-Bass: San Francisco. p. 290-312.
3. Preacher, K.J. and A.F. Hayes, SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments, & Computers : A Journal of the Psychonomic Society, Inc, 2004. 36(4): p. 717-31.
Anaesthesia, Critical Care & Pain Medicine
Guidelines for the management of women with severe pre-eclampsia.
Bonnet MP, Garnier M, Keita H, Compère V, Arthuis C, Raia-Barjat T, Berveiller P, Burey J, Bouvet L, Bruyère M, Castel A, Clouqueur E, Gonzalez Estevez M, Faitot V, Fischer C, Fuchs F, Lecarpentier E, Le Gouez A, Rigouzzo A, Rossignol M, Simon E, Vial F, Vivanti AJ, Zieleskiewicz L, Camilleri C, Sénat MV, Schmitz T, Sentilhes L. | Anaesth Crit Care Pain Med. 2021 Oct;40(5):100901
DOI: https://doi.org/10.1016/j.accpm.2021.100901
Keywords: Guidelines; Maternal morbidity; Neonatal morbidity; Severe pre-eclampsia.
Guidelines
Introduction : To provide national guidelines for the management of women with severe pre-eclampsia.
Design: A consensus committee of 26 experts was formed. A formal conflict-of-interest (COI) policy was developed at the onset of the process and enforced throughout. The entire guidelines process was conducted independently of any industrial funding. The authors were advised to follow the principles of the Grading of Recommendations Assessment, Development and Evaluation (GRADE®) system to guide assessment of quality of evidence. The potential drawbacks of making strong recommendations in the presence of low-quality evidence were emphasised.
Méthode : The last SFAR and CNGOF guidelines on the management of women with severe pre-eclampsia were published in 2009. The literature is now sufficient for an update. The aim of this expert panel guidelines is to evaluate the impact of different aspects of the management of women with severe preeclampsia on maternal and neonatal morbidities separately. The experts studied questions within 7 domains. Each question was formulated according to the PICO (Patients Intervention Comparison Outcome) model and the evidence profiles were produced. An extensive literature review and recommendations were carried out and analysed according to the GRADE® methodology.
Résultats : The SFAR/CNGOF experts panel provided 25 recommendations: 8 have a high level of evidence (GRADE 1+/-), 9 have a moderate level of evidence (GRADE 2+/-), and for 7 recommendations, the GRADE method could not be applied, resulting in expert opinions. No recommendation was provided for 3 questions. After one scoring round, strong agreement was reached between the experts for all the recommendations.
Conclusion : There was strong agreement among experts who made 25 recommendations to improve practices for the management of women with severe pre-eclampsia.
Conclusion (proposition de traduction) : Il y avait un fort accord parmi les experts qui ont fait 25 recommandations pour améliorer les pratiques de prise en charge des femmes présentant une pré-éclampsie sévère.
Commentaire :  Algorithme pour la gestion de l'hypertension artérielle chez les femmes présentant une pré-éclampsie sévère
Algorithme pour la gestion de l'hypertension artérielle chez les femmes présentant une pré-éclampsie sévère
 Protocole d'administration IV du labétolol, de la nicardipine et de l'urapidil.
Protocole d'administration IV du labétolol, de la nicardipine et de l'urapidil.
Pour information, modification de l'AMM de la nicardipine en avril 2015 :
Les indications thérapeutiques recommandées de la nicardipine par voie intraveineuse sont désormais les suivantes :
• Traitement de l’hypertension aiguë menaçant le pronostic vital, en particulier en cas de :
1. Hypertension artérielle maligne/encéphalopathie hypertensive.
2. Dissection aortique, quand le traitement par des bêta-bloquants à courte durée d’action n’est pas approprié, ou en association avec un bêta-bloquant quand le blocage des récepteurs bêta seul n’est pas efficace.
3. Pré-éclampsie sévère, quand d’autres agents antihypertenseurs administrés par voie intraveineuse ne sont pas recommandés ou sont contre-indiqués.
4. Traitement de l’hypertension post-opératoire.
Compte tenu de données disponibles insuffisantes, l’utilisation de la nicardipine n’est plus indiquée :
• En anesthésie, pour traiter l’hypotension contrôlée et l’hypertension en période péri-opératoire.
• Pour traiter l’hypertension accompagnée d'une atteinte viscérale menaçant le pronostic vital à très court terme (urgence hypertensive), notamment lors de décompensation ventriculaire gauche avec oedème pulmonaire.
Par ailleurs, la nicardipine doit être administrée uniquement en perfusion intraveineuse continue, à l’aide d’un pousse-seringue électronique ou d’une pompe volumétrique, par des spécialistes dans un environnement médical bien contrôlé, tel que les hôpitaux et unités de soins intensifs, avec une surveillance continue de la pression artérielle.
Chez les adultes, le traitement doit commencer par une administration continue de nicardipine à la vitesse de 3-5 mg/h pendant 15 min. La vitesse peut être augmentée par palier de 0,5 ou 1 mg toutes les 15 minutes, sans dépasser 15 mg/h. La nicardipine doit être utilisée avec précaution et à des doses plus faibles dans certaines populations particulières, notamment les femmes enceintes…
Annals of Emergency Medicine
What Is the Efficacy of Probiotics for the Treatment of Acute Infectious Diarrhea?.
Gottlieb M, Mogni B, Ramsay N. | Ann Emerg Med. 2021 Oct;78(4):515-516
DOI: https://doi.org/10.1016/j.annemergmed.2021.02.005
| Télécharger l'article au format
Keywords: Aucun
Infectious Disease
Introduction : The authors searched the trials register in the Cochrane Infectious Diseases Group, MEDLINE, and Embase databases from inception to December 17, 2019. The authors also reviewed existing reviews of this topic and the reference lists for any applicable trials. There were no language restrictions.
Méthode : Two independent reviewers screened studies for inclusion with discrepancies resolved by discussion. Included studies were limited to randomized controlled trials comparing a probiotic agent with either a placebo or no probiotic, in patients with acute diarrhea (duration <14 days) that was proven or assumed to be from an infectious etiology. The authors did not restrict the age group and included studies regardless of blinding. Studies of diarrhea known or thought to have an alternate etiology (eg, antibiotic-associated diarrhea, persistent diarrhea), as well as those using fermented foods (eg, yogurt) in which probiotic organisms were not identified or not active, were excluded. The primary outcomes were diarrhea lasting more than 48 hours and the duration of diarrhea. The secondary outcomes were the number of people hospitalized in community studies, duration of hospitalization in inpatient studies, diarrhea lasting more than 14 days, and adverse events.
Résultats : Three reviewers independently extracted data into a standardized form. The authors pooled the data and calculated the risk ratios (RRs) with 95% confidence intervals (CIs) for dichotomous outcomes and weighted mean differences (WMDs) for continuous outcomes. The Cochrane Risk of Bias assessment tool was used to determine study quality.1 The authors used the GRADE approach for assessing the certainty of evidence.2 The authors assessed heterogeneity with the chi-square test and I2 test. When significant heterogeneity was present, the authors used a random-effects model. In all other instances, the authors used a fixed-effects model. The authors evaluated for publication bias using a funnel plot. The authors performed a sensitivity analysis of studies deemed at low risk of bias for all categories.
Conclusion : According to studies with a low risk of bias, probiotics do not reduce the number of people having diarrhea for more than 48 hours.
Conclusion (proposition de traduction) : Selon des études à faible risque de biais, les probiotiques ne réduisent pas le nombre de personnes ayant la diarrhée pendant plus de 48 heures.
Electrocardiographic Diagnosis of Acute Coronary Occlusion Myocardial Infarction in Ventricular Paced Rhythm Using the Modified Sgarbossa Criteria.
Dodd KW, Zvosec DL, Hart MA, Glass G 3rd, Bannister LE, Body RM, Boggust BA, Brady WJ, Chang AM, Cullen L, Gómez-Vicente R, Huis In 't Veld MA, Karim RM, Meyers HP 3rd, Miranda DF, Mitchell GJ, Reynard C, Rice C, Salverda BJ, Stellpflug SJ, Tolia VM, Walsh BM, White JL, Smith SW; PERFECT study investigators. | Ann Emerg Med. 2021 Oct;78(4):517-529
DOI: https://doi.org/10.1016/j.annemergmed.2021.03.036
Keywords: Aucun
Cardiology
Introduction : Ventricular paced rhythm is thought to obscure the electrocardiographic diagnosis of acute coronary occlusion myocardial infarction. Our primary aim was to compare the sensitivity of the modified Sgarbossa criteria (MSC) to that of the original Sgarbossa criteria for the diagnosis of occlusion myocardial infarction in patients with ventricular paced rhythm.
Méthode : In this retrospective case-control investigation, we studied adult patients with ventricular paced rhythm and symptoms of acute coronary syndrome who presented in an emergency manner to 16 international cardiac referral centers between January 2008 and January 2018. The occlusion myocardial infarction group was defined angiographically as thrombolysis in myocardial infarction grade 0 to 1 flow or angiographic evidence of coronary thrombosis and peak cardiac troponin I ≥10.0 ng/mL or troponin T ≥1.0 ng/mL. There were 2 control groups: the "non-occlusion myocardial infarction-angio" group consisted of patients who underwent coronary angiography for presumed type I myocardial infarction but did not meet the definition of occlusion myocardial infarction; the "no occlusion myocardial infarction" control group consisted of randomly selected emergency department patients without occlusion myocardial infarction.
Résultats : There were 59 occlusion myocardial infarction, 90 non-occlusion myocardial infarction-angio, and 102 no occlusion myocardial infarction subjects (mean age, 72.0 years; 168 [66.9%] men). For the diagnosis of occlusion myocardial infarction, the MSC were more sensitive than the original Sgarbossa criteria (sensitivity 81% [95% confidence interval [CI] 69 to 90] versus 56% [95% CI 42 to 69]). Adding concordant ST-depression in V4 to V6 to the MSC yielded 86% (95% CI 75 to 94) sensitivity. For the no occlusion myocardial infarction control group of ED patients, additional test characteristics of MSC and original Sgarbossa criteria, respectively, were as follows: specificity 96% (95% CI 90 to 99) versus 97% (95% CI 92 to 99); negative likelihood ratio (LR) 0.19 (95% CI 0.11 to 0.33) versus 0.45 (95% CI 0.34 to 0.65); and positive LR 21 (95% CI 7.9 to 55) versus 19 (95% CI 6.1 to 59). For the non-occlusion myocardial infarction-angio control group, additional test characteristics of MSC and original Sgarbossa criteria, respectively, were as follows: specificity 84% (95% CI 76 to 91) versus 90% (95% CI 82 to 95); negative LR 0.22 (95% CI 0.13 to 0.38) versus 0.49 (95% CI 0.35 to 0.66); and positive LR 5.2 (95% CI 3.2 to 8.6) versus 5.6 (95% CI 2.9 to 11).
Conclusion : For the diagnosis of occlusion myocardial infarction in the presence of ventricular paced rhythm, the MSC were more sensitive than the original Sgarbossa criteria; specificity was high for both rules. The MSC may contribute to clinical decisionmaking for patients with ventricular paced rhythm.
Conclusion (proposition de traduction) : Pour le diagnostic d'infarctus du myocarde par occlusion coronaire en présence d'un rythme ventriculaire électroentraîné, les critères de Sgarbossa modifiés étaient plus sensibles que les critères de Sgarbossa d'origine ; la spécificité était élevée pour les deux règles. Les critères de Sgarbossa modifiés peuvent contribuer à la prise de décision clinique pour les patients présentant un rythme ventriculaire électroentraîné.
Commentaire :  Schémas des critères de Sgarbossa originaux et modifiés.
Schémas des critères de Sgarbossa originaux et modifiés.
A-C, original Sgarbossa criteria. D-F, MSC. A, Concordant ST- segment elevation (STE) more than 1 mm. B, Concordant ST-segment depression (STD) more than 1 mm. C, Discordant STE more than 5 mm. D, Concordant STE more than 1 mm. E, Concordant STD more than 1 mm. F, Discordant STE with ST-segment to S-wave ratio more than 25%. STD, ST-segment depression; STE, ST-segment elevation.
Supplemental Materials
BMC Emergency Medicine
Isolated calf deep venous thrombosis: frequency on venous ultrasound and clinical characteristics - This is part of 1 collection.
Heller T, Becher M, Kröger JC, Beller E, Heller S, Höft R, Weber MA, Meinel FG. | BMC Emerg Med. 2021 Oct 30;21(1):126
DOI: https://doi.org/10.1186/s12873-021-00516-1
| Télécharger l'article au format
Keywords: Compression ultrasound; Deep venous thrombosis; Duplex ultrasound.
Research article
Introduction : It remains controversial whether to include calf veins in the initial ultrasound evaluation of suspected deep venous thrombosis (DVT). We sought to investigate the frequency and clinical characteristics of isolated calf DVT.
Méthode : In this retrospective analysis, we investigated a cohort of 596 patients (median age 69 years, 52.3% women) who had been imaged with complete lower extremity venous duplex ultrasound for suspected acute DVT. Radiology reports were analyzed for the presence and localization of DVT. Clinical information was collected from patients' electronic charts.
Résultats : DVT was found in 157 patients (26.3%), of which 74 patients (47.1%) had isolated calf DVT. Isolated calf DVTs were located in the posterior tibial veins (22 patients, 29.7%), peroneal veins (41 patients, 55.4%) and muscle veins (19 patients, 25.7%). There were no differences in age or sex between patients with isolated calf DVT and patients with proximal DVT. Isolated calf DVT was more commonly associated with leg pain (52.7% vs. 33.7%, p = 0.0234) and less commonly associated with subjective leg swelling (35.1% vs. 55.4%, p = 0.0158) and objectively measured difference in leg circumference (23% vs. 39.8%, p = 0.0268). D-Dimers were significantly lower in patients with isolated lower leg DVT (median 2.3 vs. 6.8 mg/L, p < 0.0001) compared to patients with proximal DVT.
Conclusion : Isolated calf DVT represents approximately half of DVT cases and has different clinical characteristics than proximal DVT.
Conclusion (proposition de traduction) : La thrombose veineuse profonde isolée du mollet représente environ la moitié des cas de thrombose veineuse profonde et présente des caractéristiques cliniques différentes de la thrombose veineuse profonde proximale.
Assessment of breathing in cardiac arrest: a randomised controlled trial of three teaching methods among laypersons.
Breindahl N, Granholm A, Jensen TW, Ersbøll AK, Myklebust H, Lippert F, Lippert A. | BMC Emerg Med. 2021 Oct 9;21(1):114
DOI: https://doi.org/10.1186/s12873-021-00513-4
| Télécharger l'article au format
Keywords: Abnormal breathing; Agonal breathing; Basic life support; Breathing assessment; Breathing patterns; Cardiac arrest; Education; Gasping; Randomised controlled trial; Simulation.
Research
Introduction : The aim of this trial was to compare a video- and a simulation-based teaching method to the conventional lecture-based method, hypothesizing that the video- and simulation-based teaching methods would lead to improved recognition of breathing patterns during cardiac arrest.
Méthode : In this Danish, investigator-initiated, stratified, randomised controlled trial, adult laypersons (university students, military conscripts and elderly retirees) participating in European Resuscitation Council Basic Life Support courses were randomised to receive teaching on how to recognise breathing patterns using a lecture- (usual practice), a video-, or a simulation-based teaching method. The primary outcome was recognition of breathing patterns in nine videos of actors simulating normal breathing, no breathing, and agonal breathing (three of each). We analysed outcomes using logistic regression models and present results as odds ratios (ORs) with 95% confidence intervals (CIs) and P-values from likelihood ratio tests.
Résultats : One hundred fifty-three participants were included in the analyses from February 2, 2018 through May 21, 2019 and recognition of breathing patterns was statistically significantly different between the teaching methods (P = 0.013). Compared to lecture-based teaching (83% correct answers), both video- (90% correct answers; OR 1.77, 95% CI: 1.19-2.64) and simulation-based teaching (88% correct answers; OR 1.48; 95% CI: 1.01-2.17) led to significantly more correct answers. Video-based teaching was not statistically significantly different compared to simulation-based teaching (OR 1.20; 95% CI: 0.78-1.83).
Conclusion : Video- and simulation-based teaching methods led to improved recognition of breathing patterns among laypersons participating in adult Basic Life Support courses compared to the conventional lecture-based teaching method.
Conclusion (proposition de traduction) : Les méthodes d'enseignement basées sur la vidéo et la simulation ont permis d'améliorer la reconnaissance des schémas respiratoires chez les profanes participant aux cours de réanimation de base pour adultes par rapport à la méthode d'enseignement conventionnelle basée sur des conférences.
Bulletin épidémiologique hebdomadaire
Bouisset F, Huo Yung Kai S, Dallongeville J, Moitry M, Montaye M, Biasch K, et al. . | Bull Epidémiol Hebd. 2021 Oct;(15):266-74.
DOI: http://beh.santepubliquefrance.fr/beh/2021/15/2021_15_1.html
| Télécharger l'article au format
Keywords: Acute coronary syndrome, Ischaemic heart disease, Prognosis, MONICA
Article
Introduction : Les données disponibles comparant le pronostic à long terme des différents types de syndrome coronarien aigu (SCA) sont limitées et anciennes. L’objectif de notre étude était de comparer les pronostics vitaux à court et long terme dans le SCA avec et sans sus-décalage du segment ST (SCA ST+ et SCA non-ST+) au moyen des données du registre populationnel contemporain MONICA (Multinational monitoring of trends and determinants in cardiovascular disease).
Méthode : Les sujets âgés de 35 à 74 ans, présentant un SCA inaugural au cours de l’année 2006 et habitant dans l’une des trois zones de France couverte par le registre MONICA ont été inclus (départements du Bas-Rhin, de la Haute-Garonne et Communauté urbaine de Lille). Les données sur la présentation clinique, la prise en charge et le statut vital, à court (28 jours) et long terme (10 ans), en fonction du type de SCA (SCA ST+ et SCA non-ST+) ont été recueillies.
Résultats : Un total de 1 822 sujets présentant un SCA inaugural, 1 121 (61,5%) SCA ST+ et 701 (38,5%) SCA non-ST+, ont été inclus en 1 an. À 28 jours de suivi, les taux de mortalité étaient respectivement de 6,7% et 4,7% (p=0,09) pour les SCA ST+ et non ST+. Après ajustement sur les facteurs confondants potentiels, la probabilité de décès à 28 jours était significativement inférieure pour les SCA non-ST+ (OR=0,58, IC95%: [0,36-0,94] p=0,03). À 10 ans de suivi, les taux de mortalité étaient respectivement de 19,6% et 22,8% (p=0,11) pour les SCA ST+ et non ST+. Après ajustement sur les facteurs confondants potentiels, la probabilité de décès à 10 ans n’était pas significativement différente entre les SCA ST+ et non-ST+ (HR=1,07, IC95%: [0,83-1,38] p=0,59). Au cours de la première année de suivi, le taux de mortalité global de la population était de 7,2%, puis diminuait et se stabilisait à 1,7% par an de la 2e à la 10e année au décours du SCA initial.
Conclusion (proposition de traduction) : Les SCA ST+ ont un plus mauvais pronostic vital à 28 jours que les SCA non-ST+. Cependant, à 10 ans de suivi, SCA ST+ et SCA non-ST+ ont un pronostic vital identique.
Cochrane Database of Systematic Reviews
Antibiotics for the treatment of COVID-19.
Popp M, Stegemann M, Riemer M, Metzendorf MI, Romero CS, Mikolajewska A, Kranke P, Meybohm P, Skoetz N, Weibel S. | Cochrane Database Syst Rev. 2021 Oct 22;10(10):CD015025
DOI: https://doi.org/10.1002/14651858.cd015025
| Télécharger l'article au format
Keywords: Aucun
Intervention
Introduction : The effect of antibiotics with potential antiviral and anti-inflammatory properties are being investigated in clinical trials as treatment for COVID-19. The use of antibiotics follows the intention-to-treat the viral disease and not primarily to treat bacterial co-infections of individuals with COVID-19. A thorough understanding of the current evidence regarding effectiveness and safety of antibiotics as anti-viral treatments for COVID-19 based on randomised controlled trials (RCTs) is required.
Objectives: To assess the efficacy and safety of antibiotics compared to each other, no treatment, standard of care alone, placebo, or any other active intervention with proven efficacy for treatment of COVID-19 outpatients and inpatients. SEARCH METHODS: We searched the Cochrane COVID-19 Study Register (including MEDLINE, Embase, ClinicalTrials.gov, WHO ICTRP, medRxiv, CENTRAL), Web of Science and WHO COVID-19 Global literature on coronavirus disease to identify completed and ongoing studies to 14 June 2021.
Méthode : RCTs were included that compared antibiotics with each other, no treatment, standard of care alone, placebo, or another proven intervention, for treatment of people with confirmed COVID-19, irrespective of disease severity, treated in the in- or outpatient settings. Co-interventions had to be the same in both study arms. We excluded studies comparing antibiotics to other pharmacological interventions with unproven efficacy.
Data collection and analysis: We assessed risk of bias of primary outcomes using the Cochrane risk of bias tool (ROB 2) for RCTs. We used GRADE to rate the certainty of evidence for the following primary outcomes: 1. to treat inpatients with moderate to severe COVID-19: mortality, clinical worsening defined as new need for intubation or death, clinical improvement defined as being discharged alive, quality of life, adverse and serious adverse events, and cardiac arrhythmias; 2. to treat outpatients with asymptomatic or mild COVID-19: mortality, clinical worsening defined as hospital admission or death, clinical improvement defined as symptom resolution, quality of life, adverse and serious adverse events, and cardiac arrhythmias.
Résultats : We included 11 studies with 11,281 participants with an average age of 54 years investigating antibiotics compared to placebo, standard of care alone or another antibiotic. No study was found comparing antibiotics to an intervention with proven efficacy. All studies investigated azithromycin, two studies investigated other antibiotics compared to azithromycin. Seven studies investigated inpatients with moderate to severe COVID-19 and four investigated mild COVID-19 cases in outpatient settings. Eight studies had an open-label design, two were blinded with a placebo control, and one did not report on blinding. We identified 19 ongoing and 15 studies awaiting classification pending publication of results or clarification of inconsistencies. Of the 30 study results contributing to primary outcomes by included studies, 17 were assessed as overall low risk and 13 as some concerns of bias. Only studies investigating azithromycin reported data eligible for the prioritised primary outcomes. Azithromycin doses and treatment duration varied among included studies. Azithromycin for the treatment of COVID-19 compared to placebo or standard of care alone in inpatients We are very certain that azithromycin has little or no effect on all-cause mortality at day 28 compared to standard of care alone (risk ratio (RR) 0.98; 95% confidence interval (CI) 0.90 to 1.06; 8600 participants; 4 studies; high-certainty evidence). Azithromycin probably has little or no effect on clinical worsening or death at day 28 (RR 0.95; 95% CI 0.87 to 1.03; 7311 participants; 1 study; moderate-certainty evidence), on clinical improvement at day 28 (RR 0.96; 95% CI 0.84 to 1.11; 8172 participants; 3 studies; moderate-certainty evidence), on serious adverse events during the study period (RR 1.11; 95% CI 0.89 to 1.40; 794 participants; 4 studies; moderate-certainty evidence), and cardiac arrhythmias during the study period (RR 0.92; 95% CI 0.73 to 1.15; 7865 participants; 4 studies; moderate-certainty evidence) compared to placebo or standard of care alone. Azithromycin may increase any adverse events slightly during the study period (RR 1.20; 95% CI 0.92 to 1.57; 355 participants; 3 studies; low-certainty evidence) compared to standard of care alone. No study reported quality of life up to 28 days…
Conclusion : We are certain that risk of death in hospitalised COVID-19 patients is not reduced by treatment with azithromycin after 28 days. Further, based on moderate-certainty evidence, patients in the inpatient setting with moderate and severe disease probably do not benefit from azithromycin used as potential antiviral and anti-inflammatory treatment for COVID-19 regarding clinical worsening or improvement. For the outpatient setting, there is currently low-certainty evidence that azithromycin may have no beneficial effect for COVID-19 individuals. There is no evidence from RCTs available for other antibiotics as antiviral and anti-inflammatory treatment of COVID-19. With accordance to the living approach of this review, we will continually update our search and include eligible trials to fill this evidence gap. However, in relation to the evidence for azithromycin and in the context of antimicrobial resistance, antibiotics should not be used for treatment of COVID-19 outside well-designed RCTs.
Conclusion (proposition de traduction) : Nous sommes certains que le risque de décès chez les patients hospitalisés atteints de la COVID-19 n’est pas réduit par le traitement par l’azithromycine après 28 jours. De plus, selon des données probantes modérées et sûres, les patients hospitalisés atteints d’une maladie modérée et grave ne bénéficient probablement pas de l’azithromycine utilisée comme traitement antiviral et anti-inflammatoire potentiel contre la COVID-19 en ce qui concerne l’aggravation ou l’amélioration clinique. Pour ce qui est des patients ambulatoires, il existe actuellement des preuves à faible certitude que l’azithromycine pourrait n’avoir aucun effet bénéfique sur les personnes atteintes de la COVID-19. Il n’existe aucune preuve provenant des essai randomisé contrôlé pour d’autres antibiotiques comme traitement antiviral et anti-inflammatoire de la COVID-19. Conformément à l’approche évolutive de cette revue, nous mettrons continuellement à jour nos recherches et inclurons des essais éligibles pour combler ce manque de preuves. Toutefois, en ce qui concerne les données probantes sur l’azithromycine et dans le contexte de la résistance aux antimicrobiens, les antibiotiques ne devraient pas être utilisés pour le traitement de la COVID-19 en dehors d'essais contrôlés randomisés bien conçus.
Commentaire : COVID 19. Mission COREB nationale
• Prise en charge et suivi du patient hospitalisé .
• Prise en charge et suivi du patient en médecine de ville .
• Repérer et prendre en charge en EHPAD .
Versions du 10 novembre 2021.
Anticoagulants for acute ischaemic stroke.
Wang X, Ouyang M, Yang J, Song L, Yang M, Anderson CS. | Cochrane Database Syst Rev. 2021 Oct 22;10(10):CD000024
DOI: https://doi.org/10.1002/14651858.cd000024.pub5
| Télécharger l'article au format
Keywords: Aucun
Intervention
Introduction : Stroke is the third leading cause of early death worldwide. Most ischaemic strokes are caused by a blood clot blocking an artery in the brain. Patient outcomes might be improved if they are offered anticoagulants that reduce their risk of developing new blood clots and do not increase the risk of bleeding. This is an update of a Cochrane Review first published in 1995, with updates in 2004, 2008, and 2015.
Objectives: To assess the effectiveness and safety of early anticoagulation (within the first 14 days of onset) for people with acute presumed or confirmed ischaemic stroke. Our hypotheses were that, compared with a policy of avoiding their use, early anticoagulation would be associated with: • reduced risk of death or dependence in activities of daily living a few months after stroke onset; • reduced risk of early recurrent ischaemic stroke; • increased risk of symptomatic intracranial and extracranial haemorrhage; and • reduced risk of deep vein thrombosis and pulmonary embolism.
Méthode : We searched the Cochrane Stroke Group Trials Register (August 2021); the Cochrane Database of Systematic Reviews (CDSR); the Cochrane Central Register of Controlled Trials (CENTRAL; 2021, Issue 7), in the Cochrane Library (searched 5 August 2021); MEDLINE (2014 to 5 August 2021); and Embase (2014 to 5 August 2021). In addition, we searched ongoing trials registries and reference lists of relevant papers. For previous versions of this review, we searched the register of the Antithrombotic Trialists' (ATT) Collaboration, consulted MedStrategy (1995), and contacted relevant drug companies.
Selection criteria: Randomised trials comparing early anticoagulant therapy (started within two weeks of stroke onset) with control in people with acute presumed or confirmed ischaemic stroke.
Data collection and analysis: Two review authors independently selected trials for inclusion, assessed trial quality, and extracted data. We assessed the overall certainty of the evidence for each outcome using RoB1 and GRADE methods.
Résultats : We included 28 trials involving 24,025 participants. Quality of the trials varied considerably. We considered some studies to be at unclear or high risk of selection, performance, detection, attrition, or reporting bias. Anticoagulants tested were standard unfractionated heparin, low-molecular-weight heparins, heparinoids, oral anticoagulants, and thrombin inhibitors. Over 90% of the evidence is related to effects of anticoagulant therapy initiated within the first 48 hours of onset. No evidence suggests that early anticoagulation reduced the odds of death or dependence at the end of follow-up (odds ratio (OR) 0.98, 95% confidence interval (CI) 0.92 to 1.03; 12 RCTs, 22,428 participants; high-certainty evidence). Similarly, we found no evidence suggesting that anticoagulant therapy started within the first 14 days of stroke onset reduced the odds of death from all causes (OR 0.99, 95% CI 0.90 to 1.09; 22 RCTs, 22,602 participants; low-certainty evidence) during the treatment period. Although early anticoagulant therapy was associated with fewer recurrent ischaemic strokes (OR 0.75, 95% CI 0.65 to 0.88; 12 RCTs, 21,665 participants; moderate-certainty evidence), it was also associated with an increase in symptomatic intracranial haemorrhage (OR 2.47; 95% CI 1.90 to 3.21; 20 RCTs, 23,221 participants; moderate-certainty evidence). Similarly, early anticoagulation reduced the frequency of symptomatic pulmonary emboli (OR 0.60, 95% CI 0.44 to 0.81; 14 RCTs, 22,544 participants; high-certainty evidence), but this benefit was offset by an increase in extracranial haemorrhage (OR 2.99, 95% CI 2.24 to 3.99; 18 RCTs, 22,255 participants; moderate-certainty evidence).
Conclusion : Since the last version of this review, four new relevant studies have been published, and conclusions remain consistent. People who have early anticoagulant therapy after acute ischaemic stroke do not demonstrate any net short- or long-term benefit. Treatment with anticoagulants reduced recurrent stroke, deep vein thrombosis, and pulmonary embolism but increased bleeding risk. Data do not support the routine use of any of the currently available anticoagulants for acute ischaemic stroke.
Conclusion (proposition de traduction) : Depuis la dernière version de cette revue (Cochrane Database Syst Rev. 2015 Mar 12;2015(3):CD000024 ), quatre nouvelles études pertinentes ont été publiées et les conclusions restent cohérentes. Les personnes qui reçoivent un traitement anticoagulant précoce après un AVC ischémique aigu ne présentent aucun bénéfice net à court ou à long terme. Le traitement par anticoagulants a réduit les récidives d'AVC, la thrombose veineuse profonde et l'embolie pulmonaire, mais a augmenté le risque de saignement. Les données ne soutiennent pas l'utilisation systématique de l'un des anticoagulants actuellement disponibles pour l'AVC ischémique aigu.
Ultrasound guidance for arterial (other than femoral) catheterisation in adults.
Flumignan RL, Trevisani VF, Lopes RD, Baptista-Silva JC, Flumignan CD, Nakano LC. | Cochrane Database Syst Rev. 2021 Oct 12;10(10):CD013585
DOI: https://doi.org/10.1002/14651858.cd013585.pub2
Keywords: Aucun
Intervention
Introduction : Arterial vascular access is a frequently performed procedure, with a high possibility for adverse events (e.g. pneumothorax, haemothorax, haematoma, amputation, death), and additional techniques such as ultrasound may be useful for improving outcomes. However, ultrasound guidance for arterial access in adults is still under debate.
Objectives : To assess the effects of ultrasound guidance for arterial (other than femoral) catheterisation in adults.
Méthode : We searched CENTRAL, MEDLINE, Embase, LILACS, and CINAHL on 21 May 2021. We also searched IBECS, WHO ICTRP, and ClinicalTrials.gov on 16 June 2021, and we checked the reference lists of retrieved articles.
Selection criteria: Randomised controlled trials (RCTs), including cross-over trials and cluster-RCTs, comparing ultrasound guidance, alone or associated with other forms of guidance, versus other interventions or palpation and landmarks for arterial (other than femoral) guidance in adults.
Data collection and analysis: Two review authors independently performed study selection, extracted data, assessed risk of bias, and assessed the certainty of evidence using GRADE.
Résultats : We included 48 studies (7997 participants) that tested palpation and landmarks, Doppler auditory ultrasound assistance (DUA), direct ultrasound guidance with B-mode, or any other modified ultrasound technique for arterial (axillary, dorsalis pedis, and radial) catheterisation in adults. Radial artery Real-time B-mode ultrasound versus palpation and landmarks Real-time B-mode ultrasound guidance may improve first attempt success rate (risk ratio (RR) 1.44, 95% confidence interval (CI) 1.29 to 1.61; 4708 participants, 27 studies; low-certainty evidence) and overall success rate (RR 1.11, 95% CI 1.06 to 1.16; 4955 participants, 28 studies; low-certainty evidence), and may decrease time needed for a successful procedure (mean difference (MD) -0.33 minutes, 95% CI -0.54 to -0.13; 4902 participants, 26 studies; low-certainty evidence) up to one hour compared to palpation and landmarks. Real-time B-mode ultrasound guidance probably decreases major haematomas (RR 0.35, 95% CI 0.23 to 0.56; 2504 participants, 16 studies; moderate-certainty evidence). It is uncertain whether real-time B-mode ultrasound guidance has any effect on pseudoaneurysm, pain, and quality of life (QoL) compared to palpation and landmarks (very low-certainty evidence). Real-time B-mode ultrasound versus DUA One study (493 participants) showed that real-time B-mode ultrasound guidance probably improves first attempt success rate (RR 1.35, 95% CI 1.11 to 1.64; moderate-certainty evidence) and time needed for a successful procedure (MD -1.57 minutes, 95% CI -1.78 to -1.36; moderate-certainty evidence) up to 72 hours compared to DUA. Real-time B-mode ultrasound guidance may improve overall success rate (RR 1.13, 95% CI 0.99 to 1.29; low-certainty evidence) up to 72 hours compared to DUA. Pseudoaneurysm, major haematomas, pain, and QoL were not reported. Real-time B-mode ultrasound versus modified real-time B-mode ultrasound Real-time B-mode ultrasound guidance may decrease first attempt success rate (RR 0.68, 95% CI 0.55 to 0.84; 153 participants, 2 studies; low-certainty evidence), may decrease overall success rate (RR 0.93, 95% CI 0.86 to 1.01; 153 participants, 2 studies; low-certainty evidence), and may lead to no difference in time needed for a successful procedure (MD 0.04 minutes, 95% CI -0.01 to 0.09; 153 participants, 2 studies; low-certainty evidence) up to one hour compared to modified real-time B-mode ultrasound guidance…
Conclusion : Real-time B-mode ultrasound guidance may improve first attempt success rate, overall success rate, and time needed for a successful procedure for radial artery catheterisation compared to palpation, or DUA. In addition, real-time B-mode ultrasound guidance probably decreases major haematomas compared to palpation. However, we are uncertain about the evidence on major haematomas and pain for other comparisons due to very low-certainty evidence and unreported outcomes. We are also uncertain about the effects on pseudoaneurysm and QoL for axillary and dorsalis pedis arteries catheterisation. Given that first attempt success rate and pseudoaneurysm are the most relevant outcomes for people who underwent arterial catheterisation, future studies must measure both. Future trials must be large enough to detect effects, use validated scales, and report longer-term follow-up.
Conclusion (proposition de traduction) : Le guidage échographique en mode B en temps réel peut améliorer le taux de réussite de la première tentative, le taux de réussite global et le temps nécessaire pour une procédure réussie de cathétérisme de l'artère radiale par rapport à la palpation ou à l'assistance échographique Doppler. De plus, le guidage échographique en mode B en temps réel diminue probablement les hématomes majeurs par rapport à la palpation. Cependant, nous ne sommes pas certains des preuves sur les hématomes majeurs et la douleur pour d'autres comparaisons en raison de preuves de très faible certitude et de résultats non rapportés. Nous sommes également incertains quant aux effets sur le faux-anévrisme et la qualité perception du cathétérisme des artères axillaires et dorsales du pied. Étant donné que le taux de réussite à la première tentative et le faux-anévrisme sont les critères de jugement les plus pertinents pour les personnes ayant subi un cathétérisme artériel, les futures études doivent mesurer les deux. Les futurs essais doivent être suffisamment importants pour détecter les effets, utiliser des échelles validées et rendre compte d'un suivi à plus long terme.
Critical Care
The effect of the head-up position on cardiopulmonary resuscitation: a systematic review and meta-analysis.
Huang CC, Chen KC, Lin ZY, Chou YH, Chen WL, Lee TH, Lin KT, Hsieh PY, Chen CH, Chou CC, Lin YR. | Crit Care. 2021 Oct 30;25(1):376
DOI: https://doi.org/10.1186/s13054-021-03797-x
| Télécharger l'article au format
Keywords: Cardiopulmonary resuscitation; Cerebral perfusion pressure; Head-up position.
Research
Introduction : Experimental studies of head-up positioning (HUP) during cardiopulmonary resuscitation (CPR) have had some degree of conflicting published results. The current study aim was to analyze and reconcile those discrepancies in order to better clarify the effects of HUP CPR compared to conventional supine (SUP) CPR.
Méthode : Three databases (PubMed, EMBASE and Cochrane Library) were searched comprehensively (from each respective database's inception to May 2021) for articles addressing HUP CPR. The primary outcome to be observed was cerebral perfusion pressure (CerPP), and secondary outcomes were mean intracranial pressure (ICP), mean arterial pressure (MAP), coronary perfusion pressure (CoPP) and frequencies of return of spontaneous circulation (ROSC).
Résultats : Seven key studies involving 131 animals were included for analysis. Compared to SUP CPR, CerPP (MD 10.37; 95% CI 7.11-13.64; p < 0.01; I2 = 58%) and CoPP (MD 7.56; 95% CI 1.84-13.27, p = 0.01; I2 = 75%) increased significantly with HUP CPR, while ICP (MD - 13.66; 95% CI - 18.6 to -8.71; p < 0.01; I2 = 96%) decreased significantly. Combining all study methodologies, there were no significant differences detected in MAP (MD - 1.63; 95% CI - 10.77-7.52; p = 0.73; I2 = 93%) or frequency of ROSC (RR 0.9; 95% CI 0.31-2.60; p = 0.84; I2 = 65%). However, in contrast to worse outcomes in studies using immediate elevation of the head in a reverse Trendelenburg position, study outcomes were significantly improved when HUP (head and chest only) was introduced in a steady, graduated manner following a brief period of basic CPR augmented by active compression-decompression (ACD) and impedance threshold (ITD) devices.
Conclusion : In experimental models, gradually elevating the head and chest following a brief interval of circulatory priming with ACD and ITD devices can enhance CoPP, lower ICP and improve CerPP significantly while maintaining MAP. This effect is immediate, remains sustained and is associated with improved outcomes.
Conclusion (proposition de traduction) : Dans les modèles expérimentaux, l'élévation progressive de la tête et du thorax après un bref intervalle d'amorçage circulatoire avec des dispositifs actifs de compression-décompression et de seuil d'impédance peut augmenter la pression de perfusion coronarienne, abaisser la pression intracrânienne et améliorer considérablement la pression de perfusion cérébrale tout en maintenant la MAP. Cet effet est immédiat, reste soutenu et est associé à de meilleurs résultats.
Clinical spectrum and risk factors for mortality among seawater and freshwater critically ill drowning patients: a French multicenter study.
Reizine F, Delbove A, Dos Santos A, Bodenes L, Bouju P, Fillâtre P, Frérou A, Halley G, Lesieur O, Jonas M, Berteau F, Morin J, Luque-Paz D, Marnai R, Le Meur A, Aubron C, Reignier J, Tadié JM, Gacouin A. | Crit Care. 2021 Oct 24;25(1):372
DOI: https://doi.org/10.1186/s13054-021-03792-2
| Télécharger l'article au format
Keywords: ARDS; Cardiac arrest; Drowning; Freshwater; ICU; Saltwater.
Research
Introduction : Drowning is a global threat and one of the leading causes of injury around the world. The impact of drowning conditions including water salinity on patients' prognosis remains poorly explored in Intensive Care Units (ICUs) patients.
Méthode : We conducted a retrospective multicenter study on patients admitted to 14 ICUs in the west of France from January 2013 to January 2020. We first compared demographic and clinical characteristics at admission as well as clinical courses of these patients according to the salinity of drowning water. Then, we aimed to identify variables associated with 28-day survival using a Cox proportional hazard model.
Résultats : Of the 270 consecutive included patients, drowning occurred in seawater in 199 patients (73.7%) and in freshwater in 71 patients (26.3%). Day-28 mortality was observed in 55 patients (20.4%). Freshwater was independently associated with 28-day mortality (Adjusted Hazard Ratio (aHR) 1.84 [95% Confidence Interval (CI) 1.03-3.29], p = 0.04). A higher proportion of freshwater patients presented psychiatric comorbidities (47.9 vs. 19.1%; p < 0.0001) and the etiology of drowning appeared more frequently to be a suicide attempt in this population (25.7 vs. 4.2%; p < 0.0001). The other factors independently associated with 28-day mortality were the occurrence of a drowning-related cardiac arrest (aHR 11.5 [95% CI 2.51-52.43], p = 0.0017), duration of cardiopulmonary resuscitation (aHR 1.05 [95% CI 1.03-1.07], p < 0.0001) and SOFA score at day 1 (aHR 1.2 [95% CI 1.11-1.3], p < 0.0001).
Conclusion : In this large multicenter cohort, freshwater drowning patients had a poorer prognosis than saltwater drowning patients. Reasons for such discrepancies include differences in underlying psychiatric comorbidity, drowning circumstances and severities. Patients with initial cardiac arrest secondary to drowning remain with a very poor prognosis.
Conclusion (proposition de traduction) : Dans cette grande cohorte multicentrique, les patients noyés en eau douce avaient un pronostic plus sombre que les patients noyés en eau salée. Les raisons de ces écarts comprennent des différences dans la comorbidité psychiatrique sous-jacente, les circonstances de noyade et la gravité. Les patients avec un arrêt cardiaque initial secondaire à une noyade restent avec un très mauvais pronostic.
Critical Care Medicine
Stratification for Identification of Prognostic Categories In the Acute RESpiratory Distress Syndrome (SPIRES) Score.
Villar J, González-Martín JM, Ambrós A, Mosteiro F, Martínez D, Fernández L, Soler JA, Parra L, Solano R, Soro M, Del Campo R, González-Luengo RI, Civantos B, Montiel R, Pita-García L, Vidal A, Añón JM, Ferrando C, Díaz-Domínguez FJ, Mora-Ordoñez JM, Fernández MM, Fernández C, Fernández RL, Rodríguez-Suárez P, Steyerberg EW, Kacmarek RM; Spanish Initiative for Epidemiology, Stratification and Therapies of ARDS (SIESTA) Network. | Crit Care Med. 2021 Oct 1;49(10):e920-e930
DOI: https://doi.org/10.1097/ccm.0000000000005142
Keywords: Aucun
Online Clinical Investigations
Introduction : To develop a scoring model for stratifying patients with acute respiratory distress syndrome into risk categories (Stratification for identification of Prognostic categories In the acute RESpiratory distress syndrome score) for early prediction of death in the ICU, independent of the underlying disease and cause of death.
Méthode : A development and validation study using clinical data from four prospective, multicenter, observational cohorts.
Setting: A network of multidisciplinary ICUs.
Patients: One-thousand three-hundred one patients with moderate-to-severe acute respiratory distress syndrome managed with lung-protective ventilation.
Interventions : None.
Résultats : The study followed Transparent Reporting of a multivariable prediction model for Individual Prognosis Or Diagnosis guidelines for prediction models. We performed logistic regression analysis, bootstrapping, and internal-external validation of prediction models with variables collected within 24 hours of acute respiratory distress syndrome diagnosis in 1,000 patients for model development. Primary outcome was ICU death. The Stratification for identification of Prognostic categories In the acute RESpiratory distress syndrome score was based on patient's age, number of extrapulmonary organ failures, values of end-inspiratory plateau pressure, and ratio of Pao2 to Fio2 assessed at 24 hours of acute respiratory distress syndrome diagnosis. The pooled area under the receiver operating characteristic curve across internal-external validations was 0.860 (95% CI, 0.831-0.890). External validation in a new cohort of 301 acute respiratory distress syndrome patients confirmed the accuracy and robustness of the scoring model (area under the receiver operating characteristic curve = 0.870; 95% CI, 0.829-0.911). The Stratification for identification of Prognostic categories In the acute RESpiratory distress syndrome score stratified patients in three distinct prognostic classes and achieved better prediction of ICU death than ratio of Pao2 to Fio2 at acute respiratory distress syndrome onset or at 24 hours, Acute Physiology and Chronic Health Evaluation II score, or Sequential Organ Failure Assessment scale.
Conclusion : The Stratification for identification of Prognostic categories In the acute RESpiratory distress syndrome score represents a novel strategy for early stratification of acute respiratory distress syndrome patients into prognostic categories and for selecting patients for therapeutic trials.
Conclusion (proposition de traduction) : La stratification pour l'identification des catégories pronostiques dans le score Acute RESpiratory Distress Syndrome (SPIRES) représente une nouvelle stratégie pour la stratification précoce des patients présentant un syndrome de détresse respiratoire aiguë en catégories pronostiques et pour la sélection des patients pour les essais thérapeutiques.
Effect of Hyperbaric Oxygen Therapy Initiation Time in Acute Carbon Monoxide Poisoning.
Lee Y, Cha YS, Kim SH, Kim H. | Crit Care Med. 2021 Oct 1;49(10):e910-e919
DOI: https://doi.org/10.1097/ccm.0000000000005112
Keywords: Aucun
Online Clinical Investigations
Introduction : Hyperbaric oxygen therapy (HBO2) is recommended for symptomatic patients within 24-hour postcarbon monoxide poisoning. Previous studies have reported significantly better outcomes with treatment administered within 6 hours after carbon monoxide poisoning. Thus, we aimed to compare the neurocognitive outcomes according to HBO2 delay intervals.
Design: Retrospective analysis of data from our prospectively collected carbon monoxide poisoning registry.
Méthode : A single academic medical center in Wonju, Republic of Korea.
Patients : We analyzed the data of 706 patients older than 16 years treated with HBO2 with propensity score matching. Based on carbon monoxide exposure-to-HBO2 delay intervals, we classified patients into the early (control, less than or equal to 6 hr) and late (case, 6-24 hr) groups. The late group was further divided into Case-1 (6-12 hr) and Case-2 (12-24 hr) groups. We also compared mild (nonintubated) and severe (intubated) groups.
Interventions : HBO2.
Résultats : After propensity score matching, Global Deterioration Scale scores at 6 months postcarbon monoxide exposure showed significantly fewer poor outcome patients in the early than in the late group (p = 0.027). The early group had significantly fewer patients with poor outcomes than the Case-2 group (p = 0.035) at 1 month and than the Case-1 (p = 0.033) and Case-2 (p = 0.004) groups at 6 months. There were significantly more patients with poor prognoses at 6 months as treatment interval increased (p = 0.008). In the mild cohort, the early group had significantly fewer patients with poor 6-month outcomes than the late group (p = 0.033).
Conclusion : Patients who received HBO2 within 6 hours of carbon monoxide exposure had a better 6-month neurocognitive prognosis than those treated within 6-24 hours. An increase in the interval to treatment led to an increase in poor outcomes.
Conclusion (proposition de traduction) : Les patients ayant bénéficier d'une oxygénothérapie hyperbare dans les 6 heures suivant l'exposition au monoxyde de carbone avaient un meilleur pronostic neurocognitif à 6 mois que ceux traités dans les 6 à 24 heures. Une augmentation de l'intervalle jusqu'au traitement a entraîné une augmentation des mauvais résultats.
Andexanet Alfa or Prothrombin Complex Concentrate for Factor Xa Inhibitor Reversal in Acute Major Bleeding: A Systematic Review and Meta-Analysis.
Nederpelt CJ, Naar L, Krijnen P, le Cessie S, Kaafarani HMA, Huisman MV, Velmahos GC, Schipper IB. | Crit Care Med. 2021 Oct 1;49(10):e1025-e1036
DOI: https://doi.org/10.1097/ccm.0000000000005059
Keywords: Aucun
Online Review Article
Introduction : To combine evidence on andexanet alfa and prothrombin complex concentrates for factor Xa inhibitor-associated bleeding to guide clinicians on reversal strategies.
Méthode : Embase, Pubmed, Web of Science, and the Cochrane Library.
Study selection: Observational studies and randomized clinical trials studying hemostatic effectiveness of andexanet alfa or prothrombin complex concentrate for acute reversal of factor Xa inhibitor-associated hemorrhage.
Data extraction: Two independent reviewers extracted the data from the studies. Visualization and comparison of hemostatic effectiveness using Sarode et al or International Society of Thrombosis and Hemostasis Scientific and Standardization Committee criteria at 12 and 24 hours, (venous) thrombotic event rates, and inhospital mortality were performed by constructing Forest plots. Exploratory analysis using a logistic mixed model analysis was performed to identify factors associated with effectiveness and venous thromboembolic event.
Résultats : A total of 21 studies were included (andexanet: 438 patients; prothrombin complex concentrate: 1,278 patients). The (weighted) mean effectiveness for andexanet alfa was 82% at 12 hours and 71% at 24 hours. The (weighted) mean effectiveness for prothrombin complex concentrate was 88% at 12 hours and 76% at 24 hours. The mean 30-day symptomatic venous thromboembolic event rates were 5.0% for andexanet alfa and 1.9% for prothrombin complex concentrate. The mean 30-day total thrombotic event rates for andexanet alfa and prothrombin complex concentrate were 10.7% and 3.1%, respectively. Mean inhospital mortality was 23.3% for andexanet versus 15.8% for prothrombin complex concentrate. Exploratory analysis controlling for potential confounders did not demonstrate significant differences between both reversal agents.
Conclusion : Currently, available evidence does not unequivocally support the clinical effectiveness of andexanet alfa or prothrombin complex concentrate to reverse factor Xa inhibitor-associated acute major bleeding, nor does it permit conventional meta-analysis of potential superiority. Neither reversal agent was significantly associated with increased effectiveness or a higher rate of venous thromboembolic event. These results underscore the importance of randomized controlled trials comparing the two reversal agents and may provide guidance in designing institutional guidelines.
Conclusion (proposition de traduction) : Actuellement, les preuves disponibles ne soutiennent pas sans équivoque l'efficacité clinique de l'andexanet alfa ou du concentré de complexe prothrombine pour inverser les saignements majeurs aigus associés aux inhibiteurs du facteur Xa, ni ne permettent une méta-analyse conventionnelle de la supériorité potentielle. Aucun des deux agents d'inversion n'était significativement associé à une efficacité accrue ou à un taux plus élevé d'événements thromboemboliques veineux. Ces résultats soulignent l'importance des essais contrôlés randomisés comparant les deux agents d'inversion et peuvent fournir des orientations dans la conception de lignes directrices institutionnelles.
Emergency Radiology
Utility of measuring serum creatinine to detect renal compromise in ED patients receiving IV contrast-enhanced CT scan.
Bonadio W, Molyneux K, Lavine E, Jackson K, Kagen A, Legome E. | Emerg Radiol. 2021 Oct;28(5):899-902
DOI: https://doi.org/10.1007/s10140-021-01942-1
Keywords: IV contrast-enhanced CT; renal injury.
Original Article
Introduction : The objectives of this study are to determine the efficacy of a roster of clinical factors in identifying risk for renal insufficiency in emergency department (ED) patients requiring intravenous contrast-enhanced CT scan (IVCE-CT) and to help mitigate potential for developing contrast-induced nephropathy (CIN).
Méthode : A review was conducted of consecutive ED patients who received IVCE-CT during a 4-month period in our urban ED. The values of ED serum creatinine (SCr) performed were tabulated. The medical records of all patients with an elevated SCr (> 1.4 mg/dL) were reviewed to determine and correlate the presence of clinical risk factors for underlying renal insufficiency.
Résultats : During the 4-month study period, there were 2260 consecutive cases who received IVCE-CT; of these, 2250 (99.6%) had concomitant measurement of SCr. Elevated SCr occurred in 141 patients (6.2%); of these, 75 had a SCr > 2 mg/dL. In all, 139/141 (98.6%) with an elevated SCr had an underlying chronic or acute medical condition identified by medical record review which potentially compromised renal function, including chronic renal disease, diabetes mellitus, HIV infection, cancer, hypertension, congestive heart failure, sepsis/septic shock, chronic alcoholism, and sickle cell disease. Two patients with no identified risk factor each had (mildly) elevated SCr; both had a normal SCr measured post-CT scan. The total cost of performing serum basic metabolic panel to measure SCr in all patients during the 4-month study period was $94,500.
Conclusion : Elevated SCr is rarely present in ED patients without recognized risk factors who receive IVCE-CT scan. The vast majority with underlying renal insufficiency are readily identified by a review of the patient's medical history and/or clinical findings. Routine SCr measurement on all ED patients regardless of risk stratification prior to IVCE imaging is neither time nor cost-effective.
Conclusion (proposition de traduction) : La créatininémie est rarement élevée chez les patients des urgences, sans facteurs de risque connus, qui bénéficient d'un scanner avec injection intraveineuse de produit de contraste. La grande majorité des patients présentant une insuffisance rénale sous-jacente sont facilement identifiés par la recherche des antécédents médicaux et/ou par l'examen clinique du patient. La mesure en routine de la créatininémie chez tous les patients des urgences, indépendamment de la stratification du risque avant l'imagerie intraveineuse de produit de contraste, n'est ni rapide ni rentable.
Traumatic cervical spine fracture patterns on CT: a retrospective analysis at a level 1 trauma center.
Tang A, Pawar J, Bridge C, King R, Kakarmath S, Harris M, Khurana B. | Emerg Radiol. 2021 Oct;28(5):965-976
DOI: https://doi.org/10.1007/s10140-021-01952-z
Keywords: C2 fracture; CT cervical spine; Cervical spine fractures; Non-contiguous fractures.
Original Article
Introduction : The purpose of our study was to determine common acute traumatic cervical spine fracture patterns on CT cervical spine (CTCS).
Méthode : We retrospectively reviewed 1091 CTCS positive for traumatic fractures performed over a 10-year period at a level 1 trauma center. Fractures were classified by vertebral level, laterality, and anatomic location (anterior/posterior arch, body, odontoid, pedicle, facet, lateral mass, lamina, spinous process, transverse foramina, and transverse processes).
Résultats : C2 was the most commonly fractured vertebra (38% of all studies), followed by C7 (32.4%). 48.7% of studies had upper cervical spine (C1 and/or C2) fractures. 39.7% of positive studies involved > 1 vertebral level. Conditioned on fractures at one cervical level, the probability of fracture was greatest at adjacent levels with a 50% chance of sustaining a C7 fracture with C6 fracture. However, 31.3% (136) of studies with multi-level fractures had non-contiguous fractures. The most common isolated vertebral process fracture was of the transverse process, seen in 89 (8.2%) studies at a single level, 27 (2.5%) studies at multiple levels. Subaxial spine vertebral process fractures outnumbered body fractures with progressive dominance of vertebral process fracture down the spine.
Conclusion : C2 was the most commonly fractured vertebral level. Multi-level traumatic cervical spine fractures constituted 40% of our cohort, most commonly at C6/C7 and C1/C2. Although the conditional probability of concurrent fracture in studies with multi-level fractures was greatest in contiguous levels, nearly one-third of multi-level fractures involved non-contiguous fractures.
Conclusion (proposition de traduction) : C2 était le niveau vertébral le plus fréquemment fracturé. Les fractures traumatiques du rachis cervical à plusieurs niveaux représentaient 40 % de notre cohorte, le plus souvent en C6/C7 et C1/C2. Bien que la probabilité conditionnelle de fracture concomitante dans les études portant sur des fractures à plusieurs niveaux était la plus élevée dans les niveaux contigus, près d'un tiers des fractures à plusieurs niveaux impliquaient des fractures non contiguës.
Commentaire : Autre contexte, même résultat… :
Moore A, Dickerson E, Dillman JR and al. Incidence of nonconfounded post-computed tomography acute kidney injury in hospitalized patients with stable renal function receiving intravenous iodinated contrast material. Curr Probl Diagn Radiol. 2014 Sep-Oct;43(5):237-41 .
European Heart Journal
Effects of lignocaine vs. opioids on antiplatelet activity of ticagrelor: the LOCAL trial.
Fernando H, Duong T, Huynh K, Noonan J, Shaw J, Duffy SJ, Nehme Z, Smith K, Myles PS, Meikle PJ, Peter K, Stub D. | Eur Heart J. 2021 Oct 14;42(39):4025-4036
DOI: https://doi.org/10.1093/eurheartj/ehab557
| Télécharger l'article au format
Keywords: Acute coronary syndromes; Analgesia; Opioid-P2Y12 inhibitor interaction; Oral P2Y12 inhibitor treatment failure; Pharmacokinetics; Platelet reactivity.
CLINICAL RESEARCH
Introduction : We assessed the impact of intravenous fentanyl and lignocaine on the pharmacokinetics and pharmacodynamics of ticagrelor in patients with unstable angina and non-ST-elevation myocardial infarction and their procedural analgesic efficacy and safety.
Méthode : Seventy patients undergoing coronary angiography with ticagrelor loading were included in the pharmacokinetic and pharmacodynamic analyses of this randomized trial. Plasma ticagrelor levels 2 h post-loading dose were significantly lower in the fentanyl arm than in the lignocaine treatment arm (598 vs. 1008 ng/mL, P = 0.014). The area under the plasma-time curves for ticagrelor (1228 vs. 2753 ng h/mL, P < 0.001) and its active metabolite (201 vs. 447 ng h/mL, P = 0.001) were both significantly lower in the fentanyl arm. Expression of activated platelet glycoprotein IIb/IIIa receptor (2829 vs. 1426 mean fluorescence intensity, P = 0.006) and P-selectin (439 vs. 211 mean fluorescence intensity, P = 0.001) was significantly higher at 60 min in the fentanyl arm. A higher proportion of patients had high on-treatment platelet reactivity in the fentanyl arm at 60 min using the Multiplate Analyzer (41% vs. 9%, P = 0.002) and 120 min using the VerifyNow (30% vs. 3%, P = 0.003) and VASP (37% vs. 6%, P = 0.002) assays. Both drugs were well tolerated with a high level of patient satisfaction.
Conclusion : Unlike fentanyl, lignocaine does not impair the bioavailability or delay the antiplatelet effect of ticagrelor. Both drugs were well tolerated and effective with a high level of patient satisfaction for procedural analgesia. Routine procedural analgesia during percutaneous coronary intervention should be reconsidered and if performed, lignocaine is a beneficial alternative to fentanyl.
Conclusion (proposition de traduction) : Contrairement au fentanyl, la lidocaïne n'altère pas la biodisponibilité ni ne retarde l'effet antiplaquettaire du ticagrélor. Les deux médicaments ont été bien tolérés et efficaces avec un niveau élevé de satisfaction des patients pour l'analgésie procédurale. L'analgésie procédurale de routine lors d'une intervention coronarienne percutanée doit être reconsidérée et, si elle est pratiquée, la lidocaïne est une alternative bénéfique au fentanyl.
Commentaire :  The LOCAL trial
The LOCAL trial
Interactions avec d’autres médicaments et autres formes d’interaction :
Il a été observé un retard et une diminution de l’exposition aux inhibiteurs de P2Y12 par voie orale, chez des patients atteints de SCA traités par morphine pendant un traitement antiagrégant plaquettaire.
Cette interaction peut être liée à une diminution de la motilité gastro-intestinale et s’applique à tous les opioïdes. Même si les conséquences cliniques ne sont pas connues (Zhang Y, Wang N, Gu Q. Effects of morphine on P2Y(12) platelet inhibitors in patients with acute myocardial infarction: A meta-analysis. Am J Emerg Med. 2021 Mar;41:219–28 ), les données indiquent une réduction potentielle de l’efficacité des inhibiteurs de P2Y12 chez les patients co-traités avec la morphine.
European Journal of Emergency Medicine
Guidelines for the acute care of severe limb trauma patients.
Lefort H, Gil-Jardiné C, Chauvin A. | Eur J Emerg Med. 2021 Oct 1;28(5):339-340
DOI: https://doi.org/10.1097/mej.0000000000000835
Keywords: Aucun
Viewpoint
Editorial : Limb injury is a common cause of emergency department visits with subsequent outpatient treatment, surgery or admission in ICU. This year, the first French interdis- ciplinary recommendation conducted by the French Society of Anesthesiology and Critical care (SFAR) and the French Society of Emergency medicine (SFMU) on severe limb injuries was published. Although the majority of limb injuries do not have functional or vital consequences for the patient, some may have specific cri- teria of severity, assessed through each step of the care process.
Conclusion : The key points of these recommendations are the need of using Vittel criteria to assess the potential severity of a patient with major limb injuries, the systematic use of a tourniquet in presence of any sign of hemorrhage and to use antibiotic prophylaxis as soon as possible for an open fracture. In the context of severe limb trauma, CT angi- ography or whole-body exploration might be of interest.
Conclusion (proposition de traduction) : Les points clés de ces recommandations sont la nécessité d'utiliser les critères de Vittel pour évaluer la gravité potentielle d'un patient présentant des lésions majeures des membres, l'utilisation systématique d'un garrot en présence de tout signe d'hémorragie et d'utiliser une prophylaxie antibiotique dès que possible pour un fracture ouverte. Dans le cadre d'un traumatisme sévère des membres, l'angio-scanner ou l'exploration corps entier peuvent être intéressants.
Commentaire : Prise en charge des patients présentant un traumatisme sévère de membre(s) . Recommandation de pratique clinique. Société Française d’Anesthésie et de Réanimation (SFAR) et Société Française de Médecine d’Urgence (SFMU) en association avec la Société Française de Chirurgie Orthopédique et Traumatologique (SOFCOT), la Société de Chirurgie Vasculaire et Endovasculaire de Langue Française (SCVE) et le Service de Santé des Armées (SSA) - Décembre 2020
Relation between chest compression rate and depth: the ENFONCE Study.
Agostinucci JM, Weisslinger L, Marzouk N, Zouaghi H, Ekpe K, Genthillomme A, Adnet F, Guenin A, Reuter PG, Lapostolle F. | Eur J Emerg Med. 2021 Oct 1;28(5):352-354
DOI: https://doi.org/10.1097/mej.0000000000000802
Keywords: Aucun
Original Article
Introduction : Chest compressions are the cornerstone of cardiopulmonary resuscitation. The recent International Liaison Committee on Resuscitation guidelines recommend increasing the rate and the depth of chest compressions, to 100-120/min and 5-6 cm, based on theoretical arguments and observational studies. We hypothesized that an increased chest compressions rate could decrease chest compressions depth.
Méthode : Operators were asked to perform continuous chest compressions on a mannequin. Chest compressions rate and depth were collected. The ratio of chest compressions compliance to the guidelines, that is rate 100-120/min and depth 5-6 cm, was calculated.
Résultats : In total 951 sequences of chest compressions were studied. Median chest compressions rate: 114 (104-130)/min. Median chest compressions depth: 4.5 (3.4-5.3) cm. Correlation between rate and depth: low (R2 = 0.12). Chest compressions in compliance with the recommended rate: 434 (46%). Rate >120/min in 285 (30%) cases and <100/min in 223 (23%) cases. Chest compressions in compliance with the recommended depth: 286 (30%). Depth >6 cm in 50 (5%) cases and <5 cm in 621 (65%) cases. Finally, chest compressions were in compliance with the guidelines for both rate and depth in 141 (15%) cases. The ratio of chest compressions in compliance with the recommended depth significantly decreased with the increase of the rate: 40% for a rate <100/min, 32% for a rate in the target (100-120/min) and 18% for a rate >100/min (P < 0.0001).
Conclusion : The ratio of chest compressions in compliance with the recommended rate and depth was as low as 15%. The rate of chest compressions in compliance with the recommended depth significantly decreased when the chest compressions rate increased. To reach both recommended rate and depth seems illusive.
Conclusion (proposition de traduction) : Le ratio de compressions thoraciques conformes à la fréquence et à la profondeur recommandées était aussi faible que 15 %. Le taux de compressions thoraciques conformes à la profondeur recommandée diminuait significativement lorsque le taux de compressions thoraciques augmentait. Atteindre à la fois le taux et la profondeur recommandés semble illusoire.
Intensive Care Medicine
Targeted temperature management following out-of-hospital cardiac arrest: a systematic review and network meta-analysis of temperature targets.
Fernando SM, Di Santo P, Sadeghirad B, Lascarrou JB, Rochwerg B, Mathew R, Sekhon MS, Munshi L, Fan E, Brodie D, Rowan KM, Hough CL, McLeod SL, Vaillancourt C, Cheskes S, Ferguson ND, Scales DC, Sandroni C, Nolan JP, Hibbert B. | Intensive Care Med. 2021 Oct;47(10):1078-1088
DOI: https://doi.org/10.1007/s00134-021-06505-z
Keywords: Critical care medicine; Emergency medicine; Hypoxic; Ischemic brain injury; Out-of-hospital cardiac arrest; Targeted temperature management.
Systematic Review
Introduction : Targeted temperature management (TTM) may improve survival and functional outcome in comatose survivors of out-of-hospital cardiac arrest (OHCA), though the optimal target temperature remains unknown. We conducted a systematic review and network meta-analysis to investigate the efficacy and safety of deep hypothermia (31-32 °C), moderate hypothermia (33-34 °C), mild hypothermia (35-36 °C), and normothermia (37-37.8 °C) during TTM.
Méthode : We searched six databases from inception to June 2021 for randomized controlled trials (RCTs) evaluating TTM in comatose OHCA survivors. Two reviewers performed screening, full text review, and extraction independently. The primary outcome of interest was survival with good functional outcome. We used GRADE to rate our certainty in estimates.
Résultats : We included 10 RCTs (4218 patients). Compared with normothermia, deep hypothermia (odds ratio [OR] 1.30, 95% confidence interval [CI] 0.73-2.30), moderate hypothermia (OR 1.34, 95% CI 0.92-1.94) and mild hypothermia (OR 1.44, 95% CI 0.74-2.80) may have no effect on survival with good functional outcome (all low certainty). Deep hypothermia may not improve survival with good functional outcome, as compared to moderate hypothermia (OR 0.97, 95% CI 0.61-1.54, low certainty). Moderate hypothermia (OR 1.23, 95% CI 0.86-1.77) and deep hypothermia (OR 1.27, 95% CI 0.70-2.32) may have no effect on survival, as compared to normothermia. Finally, incidence of arrhythmia was higher with moderate hypothermia (OR 1.45, 95% CI 1.08-1.94) and deep hypothermia (OR 3.58, 95% CI 1.77-7.26), compared to normothermia (both high certainty).
Conclusion : Mild, moderate, or deep hypothermia may not improve survival or functional outcome after OHCA, as compared to normothermia. Moderate and deep hypothermia were associated with higher incidence of arrhythmia. Routine use of moderate or deep hypothermia in comatose survivors of OHCA may potentially be associated with more harm than benefit.
Conclusion (proposition de traduction) : L'hypothermie légère, modérée ou profonde peut ne pas améliorer la survie ou le résultat fonctionnel après un arrêt cardiaque en dehors de l'hôpital, par rapport à la normothermie. L'hypothermie modérée et profonde était associée à une incidence plus élevée d'arythmie. L'utilisation systématique de l'hypothermie modérée ou profonde chez les survivants comateux d'un arrêt cardiaque extra-hospitalier peut potentiellement être associée à plus de dommages que d'avantages.
Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021.
Evans L, Rhodes A, Alhazzani W and al.. | Intensive Care Med. 2021 Nov;47(11):1181-1247
DOI: https://doi.org/10.1007/s00134-021-06506-y
| Télécharger l'article au format
Keywords: Aucun
Guideline
Editorial : Sepsis is life-threatening organ dysfunction caused by a dysregulated host response to infection. Sepsis and septic shock are major healthcare problems, impacting millions of people around the world each year and killing between one in three and one in six of those it affects. Early identification and appropriate management in the initial hours after the development of sepsis improve outcomes.
The recommendations in this document are intended to provide guidance for the clinician caring for adult patients with sepsis or septic shock in the hospital setting. Recommendations from these guidelines cannot replace the clinician’s decision-making capability when presented with a unique patient’s clinical variables. These guidelines are intended to reflect best practice.
Conclusion : As in the previous version from 2016, the focus of these international guidelines is on the diagnosis and acute treatment measures in sepsis. The topics long-term outcome and treatment targets for rehabilitation are extensively discussed and accompanied by specific recommendations. These recommendations and the underlying studies reflect the increasing awareness about the long-term consequences of severe diseases requiring intensive medical care. This article summarizes the updates in a clearly comprehensible form.
Conclusion (proposition de traduction) : Comme dans la version précédente de 2016, ces directives internationales se concentrent sur le diagnostic et les mesures de traitement aigu dans le sepsis. Les thèmes des résultats à long terme et des objectifs de traitement pour la réadaptation sont longuement discutés et accompagnés de recommandations spécifiques. Ces recommandations et les études sous-jacentes reflètent la prise de conscience croissante des conséquences à long terme des maladies graves nécessitant des soins médicaux intensifs.
Internal and Emergency Medicine
Hypocalcemia is associated with adverse clinical course in patients with upper gastrointestinal bleeding.
Korytny A, Klein A, Marcusohn E, Freund Y, Neuberger A, Raz A, Miller A, Epstein D. | Intern Emerg Med. 2021 Oct;16(7):1813-1822
DOI: https://doi.org/10.1007/s11739-021-02671-6
Keywords: Calcium; Coagulation; Hemorrhage; Hypocalcemia; Upper gastrointestinal bleeding.
IM - ORIGINAL
Editorial : Acute non-variceal upper gastrointestinal bleeding (NV-UGIB) is associated with significant morbidity and mortality. Early and efficient risk stratification can facilitate management and improve outcomes. We aimed to determine whether the level of ionized calcium (Ca++), an essential co-factor in the coagulation cascade, is associated with the severity of bleeding and the need for advanced interventions among these patients. This was a retrospective single-center cohort study of all patients admitted due to NV-UGIB. The primary outcome was transfusion of ≥ 2 packed red blood cells, arterial embolization, or emergency surgery. Secondary outcomes included (1) transfusion of ≥ 2 packed red blood cells, (2) arterial embolization, or emergency surgery, and (3) all-cause in-hospital mortality. Multivariable logistic regression was performed to determine whether Ca++ was an independent predictor of these adverse outcomes. 1345 patients were included. Hypocalcemia was recorded in 604 (44.9%) patients. The rates of primary adverse outcome were significantly higher in the hypocalcemic group, 14.4% vs. 5.1%, p < 0.001. Secondary outcomes-multiple transfusions, need for angiography or surgery, and mortality were also increased (9.9% vs. 2.3%, p < 0.001, 5.3% vs. 2.8%, p = 0.03, and 33.3% vs. 24.7%, p < 0.001, respectively). Hypocalcemia was an independent predictor of primary and all the secondary outcomes, except mortality. Hypocalcemia in high-risk hospitalized patients with NV-UGIB is common and independently associated with adverse outcomes. Ca++ monitoring in this population may facilitate the rapid identification of high-risk patients. Trials are needed to assess whether correction of hypocalcemia will lead to improved outcomes.
Conclusion : Ca++ levels among high-risk patients hospitalized due to NV-UGIB is a prognostic marker for adverse clinical course. In this population, hypocalcemia is common and indepen- dently associated with an adverse clinical course, increased risk for multiple blood transfusions, and the need for urgent surgical or angiographic interventions. Ca++ monitoring may facilitate rapid identification of high-risk patients. The results of our study suggest the need to evaluate the effect of calcium supplements on the clinical course of patients with UGIB and reduced Ca++. Author
Conclusion (proposition de traduction) : Les taux de Ca++ chez les patients à haut risque hospitalisés en raison d'une hémorragie digestive haute non variqueuse sont un marqueur pronostique d'une évolution clinique défavorable. Dans cette population, l'hypocalcémie est courante et indépendamment associée à une évolution clinique défavorable, à un risque accru de transfusions sanguines multiples et à la nécessité d'interventions chirurgicales ou angiographiques urgentes. La surveillance du Ca++ peut faciliter l'identification rapide des patients à haut risque. Les résultats de notre étude suggèrent la nécessité d'évaluer l'effet de la supplémentation calcique sur l'évolution clinique des patients présentant une hémorragie digestive haute et une diminution du Ca++.
Association of early antibiotic therapy and in-hospital mortality in adult mild-to-moderate acute aspiration pneumonitis: a cohort study.
Aga M, Naganuma T, Ohashi Y, Matsuzawa H, Matsuzaka S, Cammack I, Yamada G, Serizawa Y. | Intern Emerg Med. 2021 Oct;16(7):1841-1848
DOI: https://doi.org/10.1007/s11739-021-02695-y
Keywords: Antibiotic therapy; Antimicrobial stewardship; Aspiration pneumonia; Aspiration pneumonitis; Pneumonitis.
IM - ORIGINAL
Introduction : Patients with aspiration pneumonitis often receive empiric antibiotic therapy despite it being due to a non-infectious, inflammatory response.
Objective: To study the benefits of early antibiotic therapy in patients with suspected aspiration pneumonitis in an acute care hospital.
Méthode : Retrospective cohort study using electronic medical records from Teine Keijinkai Hospital.
Participants: Adults aged over 18 years admitted with a diagnosis of aspiration pneumonitis to the Department of General Internal Medicine or Emergency Department between January 1, 2008, and May 31, 2019. A diagnosis of aspiration pneumonitis was defined as a documented macro-aspiration event and a chest radiograph demonstrating new radiographic infiltrates.
Main measures: Patients were classified into the "early antibiotic treatment" group and the "no or late treatment" group depending on whether they received antibiotic therapy for respiratory bacterial pathogens within 8 h of arrival. The primary outcome was in-hospital all-cause mortality. Secondary outcomes included length of hospital stay, antibiotic-free days, duration of fever, readmission within one month, and incidence of complications.
Résultats : Of the 146 patients enrolled, 52 (35.6%) did not receive early antibiotic therapy, while the remaining 94 (64.4%) did. There was no difference in in-hospital mortality rates between the groups after adjustment for potential confounding variables using Cox proportional hazards analysis (hazard ratio 2.78; 95% confidence interval, 0.57-13.50, p = 0.20). Patients in the no or late treatment group had more antibiotic-free days (p < 0.001) and a shorter length of hospital stay among survivors (p = 0.040) than did those in the early antibiotic treatment group. There were no statistically significant differences between the groups with respect to other secondary outcomes.
Conclusion : Early antibiotic therapy for acute aspiration pneumonitis was not associated with in-hospital mortality, but was associated with a longer hospital stay and prolonged use of antibiotics.
Conclusion (proposition de traduction) : L'antibiothérapie précoce dans la pneumopathie d'inhalation aigüe n'était pas associée à une surmortalité hospitalière mais était associée à un séjour hospitalier plus long et à une utilisation prolongée d'antibiotiques.
High-dose dexamethasone treatment for COVID-19 severe acute respiratory distress syndrome: a retrospective study.
Vecchié A, Batticciotto A, Tangianu F, Bonaventura A, Pennella B, Abenante A, Corso R, Grazioli S, Mumoli N, Para O, Maresca AM, Dalla Gasperina D, Dentali F. | Intern Emerg Med. 2021 Oct;16(7):1913-1919
DOI: https://doi.org/10.1007/s11739-021-02800-1
| Télécharger l'article au format
Keywords: ARDS; COVID-19; Dexamethasone; FiO2; Inflammation; PaO2; SARS-CoV-2.
M - ORIGINAL
Editorial : Low-dose dexamethasone reduces mortality in patients with coronavirus disease 2019 (COVID-19)-related acute respiratory distress syndrome (ARDS). We retrospectively analyzed the efficacy of high-dose dexamethasone in patients with COVID-19-related ARDS and evaluated factors affecting the composite outcome (death or invasive mechanical ventilation). From March 4th to April 1st 2020, 98 patients with COVID-19 pneumonia were included. Those who after at least 7 days from symptom onset presented a worsening of the respiratory function or of inflammatory biomarkers were started on intravenous high-dose dexamethasone (20 mg daily for 5 days, followed by 10 mg daily for 5 days). Most patients were males (62%) with a mean age of 69 years. Hypertension and cardiovascular disease (CVD) were prevalent. Following dexamethasone treatment, a significant improvement in PaO2/FiO2 (277.41 [178.5-374.8] mmHg vs. 146.75 [93.62-231.16] mmHg, p < 0.001), PaO2 (88.15 [76.62-112.0] mmHg vs. 65.65 [57.07-81.22] mmHg, p < 0.001), and SpO2 (96 [95-98]% vs. 94 [90-96]%, p < 0.001) was observed. A concomitant decrease in C-reactive protein and ferritin levels was found (132.25 [82.27-186.5] mg/L vs. 7.3 [3.3-24.2] mg/L and 1169 [665-2056] ng/mL vs. 874.0 [569.5-1434] ng/mL, respectively; p < 0.001 for both vs. baseline). CVD was found to increase the risk of the composite outcome (RR 7.64, 95% CI 1.24-47.06, p = 0.028). In hospitalized patients with COVID-19-related ARDS, high-dose dexamethasone rapidly improves the clinical status and decreases inflammatory biomarkers. CVD was found to increase the risk of the composite outcome. These data support the importance of randomized clinical trials with high-dose dexamethasone in COVID-19 patients.
Conclusion : In conclusion, this retrospective observational study in hospitalized patients treated with high-dose dexamethasone during the hyperinflammatory phase of COVID-19 showed a rapid and significant improvement in clinical and laboratory parameters along with a low rate of AEs. Randomized clinical trials are eagerly needed to confirm our positive, preliminary data with high-dose dexamethasone in COVID-19 patients.
Conclusion (proposition de traduction) : En conclusion, cette étude observationnelle rétrospective chez des patients hospitalisés traités par dexaméthasone à haute dose (20 mg) pendant la phase hyperinflammatoire de la COVID-19 a montré une amélioration rapide et significative des paramètres cliniques et de laboratoire ainsi qu'un faible taux d'effets indésirables. Des essais cliniques randomisés sont nécessaires rapidement pour confirmer nos données préliminaires positives avec de la dexaméthasone à forte dose chez les patients COVID-19.
Commentaire : REMED est un essai prospectif de phase II, en ouvert, contrôlé randomisé comparant l'efficacité de la dexaméthasone 20 mg vs 6 mg par jour
Role of ROX index in the first assessment of COVID-19 patients in the emergency department.
Gianstefani A, Farina G, Salvatore V, Alvau F, Artesiani ML, Bonfatti S, Campinoti F, Caramella I, Ciordinik M, Lorusso A, Nanni S, Nizza D, Nava S, Giostra F. | Intern Emerg Med. 2021 Oct;16(7):1959-1965
DOI: https://doi.org/10.1007/s11739-021-02675-2
| Télécharger l'article au format
Keywords: COVID-19; Emergency department; Pandemic; ROX index.
EM - ORIGINAL
Editorial : During the first outbreak of Coronavirus disease 2019 (COVID-19) Emergency Departments (EDs) were overcrowded. Hence, the need for a rapid and simple tool to support clinical decisions, such as the ROX index (Respiratory rate - OXygenation), defined as the ratio of peripheral oxygen saturation and fraction of inspired oxygen, to respiratory rate. The aim of the study was to evaluate the accuracy of the ROX index in predicting hospitalization and mortality in patients with a diagnosis of COVID-19 in the ED. The secondary outcomes were to assess the number of readmissions and the variations in the ROX index between the first and the second admission. This was an observational prospective monocentric study, carried out in the ED of Sant'Orsola-Malpighi Hospital in Bologna, Italy. Five hundred and fifty-four consecutive patients with COVID-19 were enrolled and the ROX index was calculated. Patients were followed until hospital discharge or death. A ROX index value < 25.7 was associated with hospitalization (area under the curve [AUC] = 0.737, 95% CI 0.696-0.779, p < 0.001). The ROX index < 22.3 was statistically related to higher 30-day mortality (AUC = 0.764, 95% CI 0.708-0.820, p < 0.001). Eight patients were discharged and returned to the ED within the subsequent 7 days, their mean ROX index was 30.3 (6.2; range 21.9-39.4) at the first assessment and 24.6 (5.5; 14.5-29.5) at the second assessment, (p = 0.012). The ROX index, together with laboratory, imaging and clinical findings, correlated with the need for hospital admission, mechanical ventilation and mortality risk in COVID-19 patients.
Conclusion : Considering what was previously mentioned, the ROX index seems to be a good combination of accuracy, non-invasivity and promptness, especially in those scenarios in which a blood gas analyzer is not available. For instance, it could be used by the triage nurse to place patients at adequate priority levels, by attributing color codes which are directly related to waiting time in the ED. For the same reasons, the Authors also suggest using the ROX index for patients having suspicious COVID-19 symptoms prior to admission to the ED, such as e,g., using pulse oximetry in the territorial health care services. The expectation is to help general practitioners to better manage outpatients by means of a common index, especially in the unfortunate hypothesis of another wave of COVID-19.
Conclusion (proposition de traduction) : Compte tenu de ce qui a été mentionné précédemment, l'index ROX semble être une bonne combinaison de précision, de non-invasivité et de rapidité, en particulier dans les scénarios dans lesquels un analyseur des gaz du sang n'est pas disponible. Par exemple, il pourrait être utilisé par l'infirmière de triage pour placer les patients à des niveaux de priorité adéquats, en leur attribuant des codes de couleur qui sont directement liés au temps d'attente aux urgences. Pour les mêmes raisons, les auteurs suggèrent également d'utiliser l'index ROX pour les patients présentant des symptômes suspects de COVID-19 avant leur admission aux urgences, comme par exemple l'utilisation de l'oxymétrie de pouls dans les services de santé territoriaux. Le but est d'aider les médecins généralistes à mieux prendre en charge les patients ambulatoires au moyen d'un index commun, notamment dans l'hypothèse malheureuse d'une nouvelle vague de COVID-19.
Commentaire : L'index ROX estime le besoin (ou le risque) d'intubation après la mise sous oxygénothérapie nasale à haut débit (type Optiflow®). Score pronostic
L'indice ROX [(SpO2/FiO2)/fréquence respiratoire] permet de prédire le succès ou l'échec du traitement d'une détresse respiratoire aiguë par oxygénothérapie à haut débit nasal (type Optiflow®) dans le cadre d'une pneumopathie. Il s'utilise donc, dans la prise en charge de l'insuffisance respiratoire aiguë (IRA) hypoxémique, comme critère de risque d’intubation (et donc, comme échec du traitement par haut débit nasal).
Roca O. et al. ont montré que chez des patients admis pour IRA hypoxémiante traités par haut débit nasal (HFNC), une valeur de l'indice > à 4,88, mesurée après 12 h de traitement, était prédictif de succès du traitement (c'est-à-dire que les patients ne nécessitaient pas une intubation).
C'est un score à surveiller toutes les unes à deux heures, pour voir si le patient s’améliore (score qui augmente) ou s’il est en train de se dégrader (score stable ou qui baisse) et ce, afin de ne pas manquer le moment où le patient pourrait nécessiter une intubation. 4 intervalles de temps sont observés à minima : 2, 6, 12 et > 12 heures. C'est un outil de chevet dynamique et facile à utiliser par tous les soignants.
Liu S. et al. ont montré que l'indice ROX pouvait aussi être utilisé chez les patients qui, après extubation, présentent une insuffisance respiratoire, pour prédire le résultat du traitement par HNFC. Il aide à définir des critères d'arrêt pour son utilisation, en espérant réduire les délais du traitement.
Zucman N. et al. ont montré que dans la COVID-19 l’indice ROX permettrait de prédire rapidement la réponse à l’HNFC. Une valeur < à 5,37 dans les 4 premières heures de mise en route de l’oxygénothérapie à haut-débit appliquée dès l’admission aux patients Covid-19 était prédictif du besoin ultérieur d’une intubation.
Calculateurs en ligne :
MDCalc .
Medicalcul .
Journal Européen des Urgences et de Réanimation
Balen F, Sablayrolles L, Houze C, Charpentier S, Gandois H, Auboiroux P-H. | JEUR. 2021 Oct 1;33:146–50
DOI: https://doi.org/10.1016/j.jeurea.2021.05.007
| Télécharger l'article au format
Keywords: Severe traumas, Vittel criteriaes, Whole Body Scan
ARTICLE ORIGINAL
Introduction : La traumatologie à haute énergie est la première cause de mortalité de l’adulte jeune. En France le score de Vittel est utilisé pour le tri pré-hospitalier de ces patients, mais est également utilisé en soins courants au sein des structures des urgences pour la prescription du scanner corps-entier. L’objectif de notre étude est d’évaluer la prévalence des atteintes sévères au scanner corps-entier réalisé d’après les critères de Vittel en Structure des Urgences.
Méthode : Nous avons conduit une étude de cohorte monocentrique rétrospective d’avril 2018 à mai 2019 au sein d’une Structure des Urgences du CHU de Toulouse. Tous les traumatisés ayant bénéficié d’un scanner corps-entier pour traumatisme à haute cinétique selon les critères de Vittel ont été inclus. Le critère de jugement principal était la présence d’une lésion post-traumatique sévère (nécessitant une chirurgie dans les 24h ou une admission en soins critiques).
Résultats : Parmi les 482 patients inclus, 109 (23 % ; Intervalle de confiance (IC) 95 %=[19–27]) présentaient des atteintes sévères et 231 (48 % ; IC95 %=[43–52]) patients présentent une lésion au scanner corps-entier. L’âge supérieur à 65 ans (OR=2,5 ; IC95 %=[1,1–5,5]), une chute supérieure à 3 mètres (OR=6,9 ; IC95 %=[2,5–19,4]), une SpO2 ≤90 % (OR=11,2 ; IC95 %=[2,9–43,3]) et une déformation de membre (OR=3,4 ; IC95 %=[1,7–6,8]) étaient associés significativement avec une atteinte sévère au scanner corps-entier.
Conclusion : Using Vittel criteriaes to prescribe a WBS for patients admitted in ED for traumas leads to diagnose 48% of injuries and 23% of severe injuries.
Conclusion (proposition de traduction) : L’utilisation des critères de Vittel en SU pour prescrire un scanner corps-entier devant un traumatisme cranio-thoraco-abdominal retrouve des lésions dans 48 % des cas et des lésions sévères dans 23 % des cas.
Commentaire : Critères de Vittel (onglet Traumatologie).
Afin de déterminer si une victime d’accident doit être considérée comme traumatisée grave et doit être pris en charge dans un centre spécialisé en traumatologie, on peut se référer aux critères suivants, proposés à Vittel en Octobre 2002. L’algorithme de Vittel est dérivé de la version de 1999 de l’algorithme de l’American College of Surgeons.
Le soustriage lié à l’utilisation de l’algorithme de Vittel n’a pas été évalué en France. Le surtriage lié à l’utilisation de cet algorithme varie de 38 à 42 %.
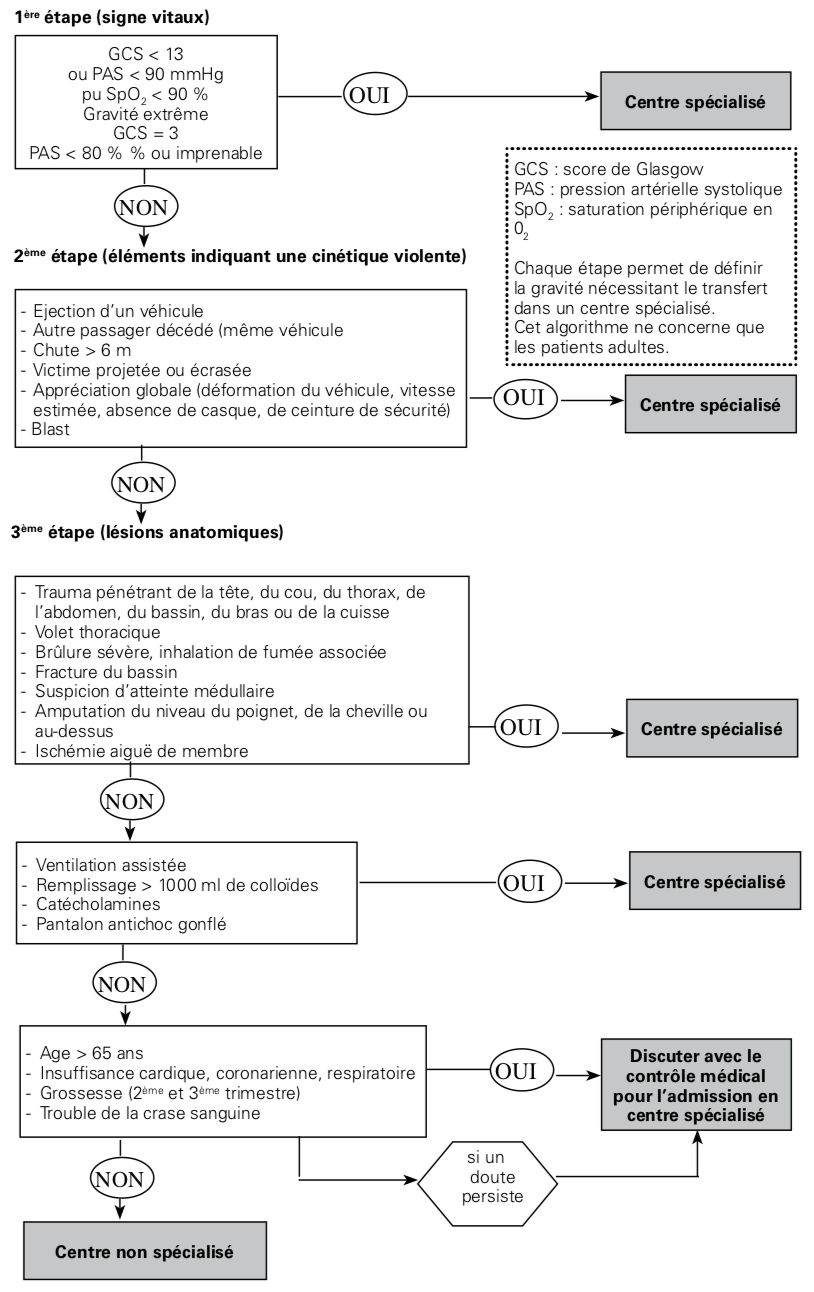
Schmitt J, Bordes J, Lacroix G, Avaro JP, Meaudre E. | JEUR. 2021;33(3):151–4.
DOI: https://doi.org/10.1016/j.jeurea.2021.06.003
| Télécharger l'article au format
Keywords: Quick Clot Combat Gauze, Damage control, Severe Trauma, Chest Trauma
Cas clinique
Editorial : La prise en charge des saignements massifs du médiastin postérieur chez les patients traumatisés sévère réside en une chirurgie de type damage control ou bien une artério embolisation. Nous rapportons le cas d’un traumatisé sévère présentant une burst fracture rachidienne compliquée d’un hémothorax massif nécessitant l’utilisation de compresses hémostatiques (Quick Clot Combat Gauze). Une telle prise en charge a déjà été décrite lors d’expériences animales ou bien exceptionnellement lors de cas cliniques. Les compresses hémostatiques pourraient être une alternative en cas d’hémostase chirurgicale difficile, mais leur usage intracorporel a besoin d’être étudié au travers d’essais randomisés contrôlés.
Conclusion (proposition de traduction) : La stratégie chirurgicale de type damage control surgery reste la pierre angulaire de la prise en charge du patient traumatisé sévère en parallèle d’une réanimation adéquate. Ce cas clinique rappelle l’utilisation du packing intracorporel par compresse hémostatique. Elle peut être une manière de stopper une exsanguination réfractaire aux moyens habituels. Pour prévenir d’éventuels effets secondaires, une reprise chirurgicale doit réévaluer le site opéré, et prodiguer une large irrigation afin de réduire le risque d’adhérence ou de brûlure. Les principales limites de leur utilisation intra corporelle semblent être une coagulopathie sévère, ainsi que les difficultés d’application liées à l’anatomie du patient. D’autres recherches sont nécessaires afin de préciser quel profil de patient pourrait bénéficier d’une telle stratégie.
Mahiou P, Darren R, Desebbe O, Rocourt F, Bouaziz H. | JEUR. 2021;33:155–61
DOI: https://doi.org/10.1016/j.jeurea.2021.09.001
| Télécharger l'article au format
Keywords: Traumatology; Hostile environment; Prehospital analgesia; Regional anesthesia; Helicopter evacuation
Article original
Editorial : Les traumatismes des sports d’aventure se produisent en environnement hostile chez des patients souvent hyperalgiques. L’anesthésie locorégionale périphérique (ALRP) en extrahospitalier a été démontrée. Néanmoins, nous nous sommes interrogés sur sa réalisation en milieu périlleux pour soulager ces douleurs sévères. Par une étude observationnelle, 19 traumatisés (six femmes, 13 hommes) ont bénéficié d’ALRP. L’évaluation s’est intéressée à sa faisabilité, aux circonstances de l’accident, aux types de traumatisme, aux EVS (de 0 à 10) à l’arrivée secours (T0), dix minutes après l’ALRP (T10), puis lors de la réduction et de l’évacuation héliportée. Quatorze accidents de ski, un de spéléologie, deux d’alpinisme, un de randonnée, et un de parapente ont été pris en charge et représentaient 11 fractures de fémur, trois de jambe, une de trois métacarpes, une luxation de rotule, et trois d’épaule. Dix-neuf ALRP ont été réalisées avec six blocs iliofasciaux, six fémoraux, trois interscaléniques, un multibloc des nerfs médian, radial, ulnaire au coude et trois sciatiques au creux poplité. Dix-sept blocs (89 %) étaient techniquement faciles et deux (11 %) difficiles. Les EVS moyenne étaient de 8 (7–9) à T0, 1 (0–2) à T10, 0,4 (0–1) à T réduction et 0,3 (0–1) à T évacuation. L’ensemble des traumatismes ont été traités sur le terrain et toutes les évacuations héliportées se sont déroulées sereinement. Les ALRP ainsi réalisées en environnement hostile sont faisables, efficaces et reproductibles sans limitation de terrain. Elles doivent être simples, rapides d’exécution et réalisées par des médecins entraînés pour obtenir un soulagement rapide de ces douleurs sévères.
Conclusion (proposition de traduction) : Les techniques ALRP sont faisables sur le terrain, même en milieu périlleux. Ces diverses techniques doivent être simples, rapides d’exécution et pratiquées par des médecins entraînés, ayant une bonne maîtrise de ces techniques d’anesthésie régionale, pour pouvoir les réaliser sur ces terrains souvent difficiles. Un des avantages majeurs est la pleine efficacité analgésique toujours supérieure à l’utilisation des diverses techniques d’analgésie sédation.
Les ALRP permettent un traitement efficace et de choix de la douleur aiguë, et autorise ainsi une réduction et une immobilisation immédiate des fractures et/ou luxations.
Plusieurs techniques d’ALRP sont à disposition en milieu extrahospitalier et milieu hostile : le BIF sans neurostimulation, ni échoguidage, le BNF avec ou sans neurostimulation en échoguidage pour la prise en charge analgésique des fractures de fémur, mais aussi le bloc du nerf sciatique au creux poplité pour les traumatismes de jambe, de cheville et du pied, et les blocs tronculaires au coude des nerfs médian, radial et ulnaire dans le cadre des fractures et/ou plaies main.
Dans l’avenir, l’utilisation adéquate de l’ALRP devra passer obligatoirement par un compagnonnage et par un apprentissage au bloc opératoire de ces diverses techniques échoguidées (diminution du risque de toxicité des AL).
La balance bénéfice/risque, quant à leurs utilisations, devra toujours être évaluée en milieu périlleux.
On n’oubliera pas d’avoir à proximité de l’intra lipide à 20 % placé dans le KIT ALRP, au cas où il serait nécessaire de traiter immédiatement une intoxication aux AL qu’il est toujours possible d’avoir sur le terrain.
Journal of Critical Care
Intubation timing as determinant of outcome in patients with acute respiratory distress syndrome by SARS-CoV-2 infection.
Vera M, Kattan E, Born P, Rivas E, Amthauer M, Nesvadba A, Lara B, Rao I, Espíndola E, Rojas L, Hernández G, Bugedo G, Castro R. | J Crit Care. 2021 Oct;65:164-169
DOI: https://doi.org/10.1016/j.jcrc.2021.06.008
| Télécharger l'article au format
Keywords: ARDS; COVID-19; Mechanical ventilation; SARS-CoV-2.
Research article - Covid 19
Introduction : To determine whether time-to-intubation was associated with higher ICU mortality in patients with COVID-19 on mechanical ventilation due to respiratory insufficiency.
Méthode : We conducted an observational, prospective, single-center study of patients with confirmed SARS-CoV-2 infection hospitalized with moderate to severe ARDS, connected to mechanical ventilation in the ICU between March 17 and July 31, 2020. We examined their general and clinical characteristics. Time-to-intubation was the time from hospital admission to endotracheal intubation.
Résultats : We included 183 consecutive patients; 28% were female, and median age was 62 years old. Eighty-eight patients (48%) were intubated before 48 h (early) and ninety-five (52%) after 48 h (late). Patients intubated early had similar admission PaO2/FiO2 ratio (123 vs 99; p = 0.179) but were younger (59 vs 64; p = 0.013) and had higher body mass index (30 vs 28; p = 0.006) compared to patients intubated late. Mortality was higher in patients intubated late (18% versus 43%), with admission PaO2/FiO2 ratio < 100 mmHg (OR 5.2; p = 0.011), of older age (OR 1.1; p = 0.001), and with previous use of ACE inhibitors (OR 4.8; p = 0.026).
Conclusion : In COVID-19 patients, late intubation, Pafi <100, older age, and previous ACE inhibitors use were associated with increased ICU mortality.
Conclusion (proposition de traduction) : Chez les patients COVID-19, l'intubation tardive, le Pafi <100, l'âge avancé et l'utilisation antérieure d' inhibiteurs de l’enzyme de conversion ont été associés à une mortalité accrue en USI.
Helmet and face mask for non-invasive respiratory support in patients with acute hypoxemic respiratory failure: A retrospective study.
Rezoagli E, Villa S, Gatti S, Russotto V, Borgo A, Lucchini A, Foti G, Bellani G. | J Crit Care. 2021 Oct;65:56-61
DOI: https://doi.org/10.1016/j.jcrc.2021.05.013
Keywords: Acute hypoxemic respiratory failure; Face mask ventilation; Helmet CPAP; Intubation; Noninvasive respiratory support.
Research article - Lung
Introduction : Non-invasive respiratory support could reduce the incidence of intubation in patients with Acute Hypoxemic Respiratory Failure (AHRF). The optimal interface or modality of non-invasive respiratory support is debated. We sought to evaluate the differences between patients who succeeded or failed non-invasive respiratory support, with a specific focus on the type of non-invasive respiratory support (i.e. helmet CPAP versus face mask NIV).
Méthode : In a single-center observational retrospective study, we investigated baseline, clinical characteristics and AHRF management by non-invasive respiratory support between January 2015 to December 2016. Data on gas exchange and respiratory mechanics, non-invasive respiratory support duration, ICU length of stay and mortality were collected.
Résultats : 110 patients with AHRF were included of which 41 patients (37%) were intubated. The use of helmet CPAP (p = 0.016) and a lower fluid balance (p = 0.038) were independently associated with a decreased rate of intubation after adjustment for confounders. Face mask NIV patients trended to a higher respiratory frequency at 1 h after treatment [28 (22-36) versus 24 (18-29) hours, p = 0.067], and showed a longer ICU stay (p = 0.009) compared to patients treated with helmet CPAP.
Conclusion : Helmet CPAP and a lower fluid balance were independent predictors of a lower intubation rate in AHRF patients in ICU. Prospective studies aimed at identifying the optimal interface and modality of non-invasive respiratory support in AHRF patients are needed.
Conclusion (proposition de traduction) : La CPAP sous casque et un bilan hydrique inférieur étaient des prédicteurs indépendants de moins d'intubation chez les patients en 'insuffisance respiratoire hypoxémique aiguë en soins intensifs. Des études prospectives visant à identifier l'interface optimale et la modalité d'assistance respiratoire non invasive chez les patients atteints d'insuffisance respiratoire hypoxémique aiguë sont nécessaires.
Journal of Intensive Care
Clinical significance of lactate clearance in patients with cardiogenic shock: results from the RESCUE registry.
Park IH, Yang JH, Jang WJ, Chun WJ, Oh JH, Park YH, Ko YG, Yu CW, Kim BS, Kim HJ, Lee HJ, Jeong JO, Gwon HC. | J Intensive Care. 2021 Oct 18;9(1):63
DOI: https://doi.org/10.1186/s40560-021-00571-7
| Télécharger l'article au format
Keywords: Cardiogenic shock; Lactate clearance; Prognosis
Research
Introduction : Limited data are available on the clinical significance of lactate clearance (LC) in patients with cardiogenic shock (CS). This study investigated the prognostic role of LC in CS patients.
Méthode : We analyzed data from 628 patients in the RESCUE registry, a multicenter, observational cohort enrolled between January 2014 and December 2018. Univariable logistic regression analysis was performed to determine the prognostic implications of 24 h LC, and then patients were divided into two groups according to the cut-off value of 24 h LC (high lactate clearance [HLC] group vs. low lactate clearance [LLC] group). The primary outcome was in-hospital mortality. We also assessed all-cause mortality at 12 month follow-up and compared the prognostic performance of 24 h LC according to initial serum lactate level.
Résultats : In the univariable logistic regression analysis, 24 h LC was associated with in-hospital mortality (odds ratio 0.989, 95% confidence interval [CI] 0.985-0.993, p < 0.001), and the cut-off value for the LC of the study population was 64%. The HLC group (initial 24 h LC ≥ 64%, n = 333) had a significantly lower incidence of in-hospital death than the LLC group (n = 295) (25.5% in the HLC group vs. 42.7% in the LLC group, p < 0.001). During 12 months of follow-up, the cumulative incidence of all-cause death was significantly lower in the HLC group than in the LLC group (33.0% vs. 48.8%; hazard ratio 0.55; 95% CI 0.42-0.70; p < 0.001). In subgroup analysis, 24 h LC predicted in-hospital mortality better in patients with initial serum lactate > 5 mmol/L than in those with serum lactate ≤ 5 mmol/L (c-statistics of initial serum lactate > 5 mmol/L = 0.782 vs. c-statistics of initial serum lactate ≤ 5 mmol/L = 0.660, p = 0.011).
Conclusion : Higher LC during the early phase of CS was associated with reduced risk of in-hospital and 12 month all-cause mortalities. Patients with LC ≥ 64% during the 24 h after CS onset could expect a favorable prognosis, especially those with an initial serum lactate > 5 mmol/L.
Conclusion (proposition de traduction) : Une clairance plus élevée du lactate au cours de la phase précoce du choc cardiogénique était associée à un risque réduit de mortalité à l'hôpital et à 12 mois toutes causes confondues. Les patients avec une clairance du lactate ≥ 64% au cours des 24 h après le début du choc cardiogénique pouvaient s'attendre à un pronostic favorable, en particulier ceux avec un lactate sérique initial > 5 mmol/L.
Journal of Intensive Care Medicine
Etomidate, Adrenal Insufficiency and Mortality Associated With Severity of Illness: A Meta-Analysis.
Albert SG, Sitaula S. | J Intensive Care Med. 2021 Oct;36(10):1124-1129
DOI: https://doi.org/10.1177/0885066620957596
Keywords: adrenal insufficiency; corticosteroids; critical care; critical illness related corticosteroid insufficiency (CIRCI); etomidate; glucocorticoid; intensive care.
Analytic Reviews
Introduction : Etomidate causes adrenal insufficiency. Yet in critically ill patients, it is controversial whether it increases mortality rates above that of comparator anesthetic induction agents. We postulated that etomidate would increase relative mortality rates correspondingly to the severity of illness as defined by SAPS or APACHE scores.
Méthode : A literature search was performed on Pub Med, SCOPUS, and Cochrane Reviews for human studies, regardless of language, between 1983 and February 2020. The search strategy used keywords, "etomidate," "adrenal insufficiency," "glucocorticoid," and "intensive care." Both authors reviewed electronic data search titles, abstracts and extracted data, which were checked by the other reviewer. Primary outcome was 28-day survival. Secondary outcome was adrenal insufficiency.
Résultats : There were 29 trials of etomidate versus comparators in 8584 patients. Etomidate was associated with adrenal insufficiency (risk ratio (rr) = 1·54, 95% CI; 1·42, 1·67, p < 0.001) and increased overall relative mortality rates (rr = 1.09, CI;1.04,1.16, p = 0.001). Meta-regression showed that with etomidate there was a continuous progressive relative risk of mortality associated with increasing severity of illness (predefined in each article by standard critical illness scores). In those patients who had a predicted mortality rate > the median for this analysis (predicted mortality 44%) the relative mortality rate (rr) = 1.20, Ci;1.12,1.29, p < 0.001, the absolute risk difference (rd) = 0.08, CI;0.05,0.11, p < 0.0001 and the number needed to harm (1/rd) was 12.5. In those with a calculated predicted mortality <44% there was no increase in relative mortality rate.
Conclusion : Whereas etomidate causes adrenal insufficiency, it was not shown to increase mortality in many analyzed here in ICU settings. However, etomidate associated relative mortality rates increased progressively and correlated with the severity of critical illness scores. Intensivists should anticipate the need for glucocorticoid supplementation after etomidate in those with severe critical illness and in those with acute deterioration of vital signs.
Conclusion (proposition de traduction) : Alors que l'étomidate provoque une insuffisance surrénale, il n'a pas été démontré qu'il augmentait la mortalité dans de nombreux cas analysés ici, en soins intensifs. Cependant, les taux de mortalité relatifs associés à l'étomidate ont augmenté progressivement et se sont corrélés avec la gravité des scores gravités. Les réanimateurs doivent anticiper la nécessité d'une supplémentation en glucocorticoïdes après l'administration d'étomidate chez les patients présentant une maladie grave grave et chez ceux présentant une détérioration aiguë des signes vitaux.
Journal of the American College of Cardiology
2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR Guideline for the Evaluation and Diagnosis of Chest Pain: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines.
Writing Committee Members, Gulati M, Levy PD, Mukherjee D, Amsterdam E, Bhatt DL, Birtcher KK, Blankstein R, Boyd J, Bullock-Palmer RP, Conejo T, Diercks DB, Gentile F, Greenwood JP, Hess EP, Hollenberg SM, Jaber WA, Jneid H, Joglar JA, Morrow DA, O'Connor RE, Ross MA, Shaw LJ. | J Am Coll Cardiol. 2021 Nov 30;78(22):e187-e285
DOI: https://doi.org/10.1016/j.jacc.2021.07.053
| Télécharger l'article au format
Keywords: ACC/AHA Clinical Practice Guidelines; accelerated diagnostic pathway; acute coronary syndrome; angina; biomarkers; cardiac imaging; chest pain; chest pain syndromes; clinical decision pathway; coronary artery disease; myocardial infarction; myocardial injury; myocardial ischemia; noncardiac; noncardiac chest pain; sex differences; shared decision-making; troponins.
Clinical Practice Guideline
Introduction : This clinical practice guideline for the evaluation and diagnosis of chest pain provides recommendations and algorithms for clinicians to assess and diagnose chest pain in adult patients.A comprehensive literature search was conducted from November 11, 2017, to May 1, 2020, encompassing randomized and nonrandomized trials, observational studies, registries, reviews, and other evidence conducted on human subjects that were published in English from PubMed, EMBASE, the Cochrane Collaboration, Agency for Healthcare Research and Quality reports, and other relevant databases. Additional relevant studies, published through April 2021, were also considered.
Conclusion : Chest pain is a frequent cause for emergency department visits in the United States. The "2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR Guideline for the Evaluation and Diagnosis of Chest Pain" provides recommendations based on contemporary evidence on the assessment and evaluation of chest pain. This guideline presents an evidence-based approach to risk stratification and the diagnostic workup for the evaluation of chest pain. Cost-value considerations in diagnostic testing have been incorporated, and shared decision-making with patients is recommended.
Conclusion (proposition de traduction) : La douleur thoracique est une cause fréquente de consultation aux urgences aux États-Unis. La « Recommandation 2021 de l'AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR pour l'évaluation et le diagnostic de la douleur thoracique » fournit des recommandations basées sur des preuves contemporaines sur l'évaluation et l'évaluation de la douleur thoracique. Cette ligne directrice présente une approche fondée sur des preuves pour la stratification du risque et le bilan diagnostique pour l'évaluation de la douleur thoracique. Des considérations de coût-valeur dans les tests de diagnostic ont été intégrées, et la prise de décision partagée avec les patients est recommandée.
Commentaire : Voir l'analyse de l'article sur le site Medscape : Chest Pain Clinical Practice Guidelines (ACC/AHA, 2021) . Rédigé le December 03, 2021.
Journal of the American Medical Association
Effect of Vasopressin and Methylprednisolone vs Placebo on Return of Spontaneous Circulation in Patients With In-Hospital Cardiac Arrest: A Randomized Clinical Trial.
Andersen LW, Isbye D, Kjærgaard J, Kristensen CM, Darling S, Zwisler ST, Fisker S, Schmidt JC, Kirkegaard H, Grejs AM, Rossau JRG, Larsen JM, Rasmussen BS, Riddersholm S, Iversen K, Schultz M, Nielsen JL, Løfgren B, Lauridsen KG, Sølling C, Pælestik K, Kjærgaard AG, Due-Rasmussen D, Folke F, Charlot MG, Jepsen RMHG, Wiberg S, Donnino M, Kurth T, Høybye M, Sindberg B, Holmberg MJ, Granfeldt A.. | JAMA. 2021 Oct 26;326(16):1586-1594
DOI: https://doi.org/10.1001/jama.2021.16628
Keywords: Aucun
Original Investigation
Introduction : Previous trials have suggested that vasopressin and methylprednisolone administered during in-hospital cardiac arrest might improve outcomes.
Objective: To determine whether the combination of vasopressin and methylprednisolone administered during in-hospital cardiac arrest improves return of spontaneous circulation.
Méthode : Multicenter, randomized, double-blind, placebo-controlled trial conducted at 10 hospitals in Denmark. A total of 512 adult patients with in-hospital cardiac arrest were included between October 15, 2018, and January 21, 2021. The last 90-day follow-up was on April 21, 2021.
Intervention: Patients were randomized to receive a combination of vasopressin and methylprednisolone (n = 245) or placebo (n = 267). The first dose of vasopressin (20 IU) and methylprednisolone (40 mg), or corresponding placebo, was administered after the first dose of epinephrine. Additional doses of vasopressin or corresponding placebo were administered after each additional dose of epinephrine for a maximum of 4 doses.
Main outcomes and measures: The primary outcome was return of spontaneous circulation. Secondary outcomes included survival and favorable neurologic outcome at 30 days (Cerebral Performance Category score of 1 or 2).
Résultats : Among 512 patients who were randomized, 501 met all inclusion and no exclusion criteria and were included in the analysis (mean [SD] age, 71 [13] years; 322 men [64%]). One hundred of 237 patients (42%) in the vasopressin and methylprednisolone group and 86 of 264 patients (33%) in the placebo group achieved return of spontaneous circulation (risk ratio, 1.30 [95% CI, 1.03-1.63]; risk difference, 9.6% [95% CI, 1.1%-18.0%]; P = .03). At 30 days, 23 patients (9.7%) in the intervention group and 31 patients (12%) in the placebo group were alive (risk ratio, 0.83 [95% CI, 0.50-1.37]; risk difference: -2.0% [95% CI, -7.5% to 3.5%]; P = .48). A favorable neurologic outcome was observed in 18 patients (7.6%) in the intervention group and 20 patients (7.6%) in the placebo group at 30 days (risk ratio, 1.00 [95% CI, 0.55-1.83]; risk difference, 0.0% [95% CI, -4.7% to 4.9%]; P > .99). In patients with return of spontaneous circulation, hyperglycemia occurred in 77 (77%) in the intervention group and 63 (73%) in the placebo group. Hypernatremia occurred in 28 (28%) and 27 (31%), in the intervention and placebo groups, respectively.
Conclusion : Among patients with in-hospital cardiac arrest, administration of vasopressin and methylprednisolone, compared with placebo, significantly increased the likelihood of return of spontaneous circulation. However, there is uncertainty whether this treatment results in benefit or harm for long-term survival.
Conclusion (proposition de traduction) : Chez les patients ayant subi un arrêt cardiaque à l'hôpital, l'administration de vasopressine et de méthylprednisolone, par rapport au placebo, a significativement augmenté la probabilité de retour à une activité circulatoire spontanée. Cependant, il existe une incertitude quant à savoir si ce traitement entraîne des avantages ou des inconvénients pour la survie à long terme.
Le Praticien en Anesthésie Réanimation
Seytre NA, Nguyen P, Salvib N. | Prat Anesth rea. 2021 October;25(5):240-247
DOI: https://doi.org/10.1016/j.pratan.2021.09.007
Keywords: Administration; Intravenous pain; Procedural vascular; Access device peripheral; Venous access; Difficult venous access; Pediatric anesthesia
Mise au point
Editorial : La pose de voie veineuse périphérique est un geste essentiel dans la prise en charge hospitalière pédiatrique. Déjà potentiellement douloureuse pour l’enfant, sa réalisation est intrinsèquement difficile pour le soignant avec un taux d’échec global de 14 %, dont 25 à 47 % lors de la première ponction. Dans cet article, nous établissons d’abord un état des connaissances sur le sujet, tant en termes de technique d’abord veineux que de stratégie antalgique. Nous proposons ensuite un algorithme de prise en charge avec identification des patients difficiles et incrémentation des techniques.
Conclusion (proposition de traduction) : La pose de VVP, bien que très fréquente en pédiatrie, nécessite une approche globale de l’enfant : de la décision médicale au succès de mise en place avec l’administration médicamenteuse souhaitée.
Nous avons fait l’état des lieux des connaissances concernant la prise en charge de la douleur induite par les soins en pédiatrie et sur les différentes techniques et dispositifs permettant d’améliorer le taux de succès lors de la mise en place d’une VVP. Malheureusement, aucun dispositif ne permet à lui seul de résoudre la difficulté technique inhérente à ce geste, surtout chez l’enfant de moins de deux ans.
La poursuite d’une stratégie systématisée peut permettre d’améliorer la prise en charge individuelle des enfants et d’améliorer la fluidité des flux de patients en développant le recours précoce à des techniques expertes telles que l’échographie, la transillumination infrarouge et l’hypnose thérapeutique.
Commentaire :  Proposition d’algorithme de perfusion à destination des services de pédiatrie.
Proposition d’algorithme de perfusion à destination des services de pédiatrie.
Pediatric Emergency Care
Comparison of Minimally Invasive Loop Drainage and Standard Incision and Drainage of Cutaneous Abscesses in Children Presenting to a Pediatric Emergency Department: A Prospective, Randomized, Noninferiority Trial.
Rencher L, Whitaker W, Schechter-Perkins E, Wilkinson M. | Pediatr Emerg Care. 2021 Oct 1;37(10):e615-e620
DOI: https://doi.org/10.1097/pec.0000000000001732
Keywords: Aucun
Original article
Introduction : This study aimed to determine whether the treatment of skin abscesses with vessel loop drainage is noninferior to standard incision and drainage (I&D) regarding treatment failure in pediatric patients in the emergency department (ED).
Méthode : This study was a prospective, randomized controlled trial in a pediatric ED of an urban tertiary pediatric hospital. Patients with a skin abscess were enrolled. Subjects were assigned to the control arm of I&D or the study arm of vessel loop drainage. Study end points (failure rates, satisfaction scores, wound appearance, visit frequency) were assessed before discharge from the ED, at 24- to 48-hour follow-up, and at 14-day follow-up. Treatment failure was declared if the abscess required reinstrumentation or admission for intravenous antibiotics for systemic illness within 14 days.
Résultats : From August 2014 to October 2015, 81 patients completed this study. Treatment failure was observed in 3 subjects of each arm (7.3% loop vs 7.5% standard; risk difference, 0.2%; 95% confidence interval, -11.2% to 11.6%). Parent satisfaction rates with wound appearance at day 14 were similar (86.1% loop vs 88.2% standard were at least satisfied). Median cosmetic scores were similar at day 14 (6 [interquartile range {IQR}, 5-6] loop vs 6 [IQR, 5-6] standard, where 6 was optimal). Follow-up visit frequency was similar (2 [IQR, 2-3] loop vs 2 [IQR, 2-2.5] standard).
Conclusion : Abscess drainage with a vessel loop in the pediatric ED results in failure rates noninferior to those of the standard I&D. Satisfaction and cosmetic scores are favorable in both groups.
Conclusion (proposition de traduction) : Le drainage en boucle d'abcès cutanés dans un service d'urgence pédiatrique entraîne des taux d'échec non inférieurs à ceux de l'incision et du drainage standard. Les scores de satisfaction et cosmétiques sont favorables dans les deux groupes.
Commentaire : Voir la technique :
Drainage en boucle d'abcès cutanés . Document proposé par TopMedecine. Juillet 2020.
Efficacy of Apneic Oxygenation During Pediatric Endotracheal Intubation.
Dancy MA | Pediatr Emerg Care. 2021 Oct 1;37(10):528-532
DOI: https://doi.org/10.1097/pec.0000000000002539
Keywords: Aucun
Review Article
Introduction : Because of the abundance of complications associated with peri-intubation hypoxia, maintaining adequate oxygen saturation during endotracheal intubation (ETI) is of great concern. In addition to standard preoxygenation techniques, apneic oxygenation (AO), the continuous flow of passive oxygenation, is a potential tool that can be used to eliminate hypoxia during ETI. Although scarcely studied in the pediatric population, AO has proven effective in reducing the incidence of hypoxia in adult patients with minimal side effects. The objective of this study is to evaluate the use of apneic oxygenation in pediatric patients and to determine its efficacy in preventing or delaying oxygen desaturation during the apneic period of ETI.
Méthode : This literature review examines 4 studies that evaluate the practice of AO in pediatric patients. A total of 712 patients across 3 randomized control trials and 1 observational study were assigned to either a control group that did not receive any form of AO, a group that did not receive 100% fraction of inspired oxygen (FiO2), or an intervention group where various methods of AO were delivered.
Résultats : Each AO method that provided 100% FiO2 saw a significantly longer time until initial desaturation when compared with those that did not receive any form of AO or those not receiving 100% FiO2.
Conclusion : The findings in this study confirm that the practice of AO is not only efficacious in increasing the time until initial desaturation but also reduces the overall incidence of hypoxia during laryngoscopy in children.
Conclusion (proposition de traduction) : Les résultats de cette étude confirment que la pratique de l'oxygénation apnéique est non seulement efficace pour augmenter le temps jusqu'à la désaturation initiale, mais réduit également l'incidence globale de l'hypoxie pendant la laryngoscopie chez les enfants.
Diagnosis and Acute Management of COVID-19 and Multisystem Inflammatory Syndrome in Children.
Kortz TB, Connolly E, Cohen CL, Cook RE, Jonas JA, Lipnick MS, Kissoon N. | Pediatr Emerg Care. 2021 Oct 1;37(10):519-525
DOI: https://doi.org/10.1097/pec.0000000000002538
Keywords: Aucun
CME Review Article
Editorial : Most children with coronavirus disease 2019 (COVID-19) infection are asymptomatic or have mild disease. About 5% of infected children will develop severe or critical disease. Rapid identification and treatment are essential for children who are critically ill with signs and symptoms of respiratory failure, septic shock, and multisystem inflammatory syndrome in children. This article is intended for pediatricians, pediatric emergency physicians, and individuals involved in the emergency care of children. It reviews the current epidemiology of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in children, summarizes key aspects of clinical assessment including identification of high-risk patients and manifestations of severe disease, and provides an overview of COVID-19 management in the emergency department based on clinical severity.
Commentaire : 
Quelques liens :
• Surveillance nationale des cas de syndrome inflammatoire multi-systémique pédiatrique (PIMS) . Santé Publique France. Mis à jour le 25 novembre 2021 ;
• Covid-19 : repérer et déclencher la prise en charge du syndrome inflammatoire multi-systémique (PIMS) de l’enfant . HAS. Mis en ligne le 08 juillet 2021 et le fichier , validée par le Collège le 1er juillet 2021 ;
• Covid-19/Prise en charge PIMS . Société Française de Pédiatrie, GFRUP. 22/03/2021.
Prehospital and Disaster Medicine
Pediatric Prehospital Advanced Airway Management by Anesthesiologist and Nurse Anesthetist Staffed Critical Care Teams.
Renberg M, Hertzberg D, Kornhall D, Günther M, Gellerfors M. | Prehosp Disaster Med. 2021 Oct;36(5):547-552
DOI: https://doi.org/10.1017/s1049023x21000637
Keywords: Aucun
Original Research
Introduction : Prehospital pediatric tracheal intubation (TI) is a possible life-saving intervention that requires adequate experience to mitigate associated complications. The pediatric airway and respiratory physiology present challenges in addition to a relatively rare incidence of prehospital pediatric TI.
tudy objectiveS: The aim of this study was to describe characteristics and outcomes of prehospital TI in pediatric patients treated by critical care teams.
Méthode : This is a sub-group analysis of all pediatric (<16 years old) patients from a prospective, observational, multi-center study on prehospital advanced airway management in the Nordic countries from May 2015 through November 2016. The TIs were performed by anesthesiologists and nurse anesthetists staffing six helicopter and six Rapid Response Car (RRC) prehospital critical care teams.
Résultats : In the study, 74 children were tracheal intubated, which corresponds to 3.7% (74/2,027) of the total number of patients. The pediatric patients were intubated by very experienced providers, of which 80% had performed ≥2,500 TIs. The overall TI success rate, first pass success rate, and airway complication rate were in all children (<16 years) 98%, 82%, and 12%. The corresponding rates among infants (<2 years) were 94%, 67%, and 11%. The median time on scene was 30 minutes.
Conclusion : This study observed a high overall prehospital TI success rate in children with relatively few associated complications and short time on scene, despite the challenges presented by the pediatric prehospital TI.
Conclusion (proposition de traduction) : Cette étude a observé un taux de réussite global élevé de l'intubation trachéale préhospitalière chez les enfants avec relativement peu de complications associées et peu de temps sur les lieux, malgré les défis présentés par l'intubation trachéale préhospitalière pédiatrique.
Development of a Performance Assessment Scale for Simulated Dispatcher-Assisted Cardiopulmonary Resuscitation (Telephone-CPR): A Multi-Center Randomized Simulation-Based Clinical Trial.
Ghazali DA, Delaire C, Blottiaux E, Lardeur JY, Jost D, Violeau M, Breque C, Oriot D. | Prehosp Disaster Med. 2021 Oct;36(5):561-569
DOI: https://doi.org/10.1017/s1049023x21000716
Keywords: bystander; cardiopulmonary resuscitation; dispatcher; simulation; telephone scale.
Original research
Introduction : Dispatchers should be trained to interrogate bystanders with strict protocols to elicit information focused on recognizing cardiac arrest and should provide telephone cardiopulmonary resuscitation (CPR) instructions in all cases of suspected cardiac arrest. While an objective assessment of training outcomes is needed, there is no performance assessment scale for simulated dispatcher-assisted CPR.
Study objective: The aim of the study was to create a valid and reliable performance assessment scale for simulated dispatcher-assisted CPR.
Méthode : In this prospective, randomized, controlled, multi-centric simulation-based trial (registration number TCTR20210130002), the scale was developed according to the European Resuscitation Council (ERC) and American Heart Association (AHA) Guidelines 2015 and revised by experts. The performance of 48 dispatchers' telephone-CPR and of 48 bystanders carrying out CPR on a manikin was assessed by two independent evaluators using the scale and using a SkillReporter (PC) software to provide CPR objective performance. Continuous variables were described as mean (SD) and categorical variables as numbers and percentage (%). Comparative analysis between two groups used a Student t-test or a non-parametric test of Mann-Whitney. The internal structure of the scale was evaluated, including internal consistency using α Cronbach coefficient, and reproducibility using intraclass correlation coefficient (ICC) and linear correlation coefficient (R2) calculation.
Résultats : The scale included three different parts: two sections for dispatchers' (32 items) and bystanders' CPR performance (15 items) assessment, and a third part recording times. There was excellent internal consistency (α Cronbach coefficient = 0.77) and reproducibility (ICC = 0.93; R² = 0.86). For dispatchers' performance assessment, α Cronbach coefficient = 0.76; ICC = 0.91; R2 = 0.84. For bystanders' performance assessment, α Cronbach coefficient = 0.75; ICC = 0.93; R2 = 0.87. Reproducibility was excellent for nine items, good for 19 items, and moderate for 19 items. No item had poor reproducibility. There was no significant difference between dispatch doctors' and medical dispatch assistants' performances (33.0 [SD = 4.7] versus 32.3 [SD = 3.2] out of 52, respectively; P = .70) or between trained and untrained bystanders to follow the instructions (14.3 [SD = 2.0] versus 13.9 [SD = 1.8], respectively; P = .64). Objective performance (%) was significantly higher for trained bystanders than for untrained bystanders (67.4 [SD = 14.5] versus 50.6 [SD = 19.3], respectively; P = .03).
Conclusion : The scale was valid and reliable to assess performance for simulated dispatcher-assisted CPR. To the authors' knowledge, no other valid performance tool currently exists. It could be used in simulated telephone-CPR training programs to improve performance.
Conclusion (proposition de traduction) : L'échelle était valide et fiable pour évaluer la performance d'une simulation de RCP mise en œuvre par un assistant de régulation. À la connaissance des auteurs, aucun autre outil de performance valide n'existe actuellement. Il pourrait être utilisé dans des programmes de formation de simulation par téléphone de la RCP pour améliorer les performances.
Commentaire : Voir le document :
• Pradeau C, Thicoipe M. Gestion téléphonique d’un appel pour arrêt cardiaque . Urgences 2011.
Resuscitation
Targeted temperature management in adult cardiac arrest: Systematic review and meta-analysis.
Granfeldt A, Holmberg MJ, Nolan JP, Soar J, Andersen LW; International Liaison Committee on Resuscitation (ILCOR) Advanced Life Support Task Force. | Resuscitation. 2021 Oct;167:160-172
DOI: https://doi.org/10.1016/j.resuscitation.2021.08.040
| Télécharger l'article au format
Keywords: Cardiac arrest; Cooling; Hypothermia; Systematic review; Targeted temperature management.
Review
Introduction : To perform a systematic review and meta-analysis on targeted temperature management in adult cardiac arrest patients.
Méthode : PubMed, Embase, and the Cochrane Central Register of Controlled Trials were searched on June 17, 2021 for clinical trials. The population included adult patients with cardiac arrest. The review included all aspects of targeted temperature management including timing, temperature, duration, method of induction and maintenance, and rewarming. Two investigators reviewed trials for relevance, extracted data, and assessed risk of bias. Data were pooled using random-effects models. Certainty of evidence was evaluated using GRADE.
Résultats : The systematic search identified 32 trials. Risk of bias was assessed as intermediate for most of the outcomes. For targeted temperature management with a target of 32-34 °C vs. normothermia (which often required active cooling), 9 trials were identified, with six trials included in meta-analyses. Targeted temperature management with a target of 32-34 °C did not result in an improvement in survival (risk ratio: 1.08 [95%CI: 0.89, 1.30]) or favorable neurologic outcome (risk ratio: 1.21 [95%CI: 0.91, 1.61]) at 90 to 180 days after the cardiac arrest (low certainty of evidence). Three trials assessed different hypothermic temperature targets and found no difference in outcomes (low certainty of evidence). Ten trials were identified comparing prehospital cooling vs. no prehospital cooling with no improvement in survival (risk ratio: 1.01 [95%CI: 0.92, 1.11]) or favorable neurologic outcome (risk ratio: 1.00 [95%CI: 0.90, 1.11]) at hospital discharge (moderate certainty of evidence).
Conclusion : Among adult patients with cardiac arrest, the use of targeted temperature management at 32-34 °C, when compared to normothermia, did not result in improved outcomes in this meta-analysis. There was no effect of initiating targeted temperature management prior to hospital arrival. These findings warrant an update of international cardiac arrest guidelines.
Conclusion (proposition de traduction) : Chez les patients adultes ayant subi un arrêt cardiaque, le contrôle ciblée de la température entre 32 et 34 °C, par rapport à la normothermie, n'a pas entraîné d'amélioration des résultats dans cette méta-analyse. Le contrôle ciblée de la température avant l'arrivée à l'hôpital n'a eu aucun effet. Ces résultats justifient une mise à jour des directives internationales dans l'arrêt cardiaque.
Prognostic association of frailty with post-arrest outcomes following cardiac arrest: A systematic review and meta-analysis.
Mowbray FI, Manlongat D, Correia RH, Strum RP, Fernando SM, McIsaac D, de Wit K, Worster A, Costa AP, Griffith LE, Douma M, Nolan JP, Muscedere J, Couban R, Foroutan F. | Resuscitation. 2021 Oct;167:242-250
DOI: https://doi.org/10.1016/j.resuscitation.2021.06.009
Keywords: Cardiac arrest; Cardiopulmonary resuscitation; Frailty; Prognosis.
Review
Introduction : To synthesize the current evidence examining the association between frailty and a series of post-arrest outcomes following the provision of cardiopulmonary resuscitation (CPR).
We searched MEDLINE, PubMed (exclusive of MEDLINE), EMBASE, CINAHL, and Web of Science from inception to August 2020 for observational studies that examined an association between frailty and post-arrest health outcomes, including in-hospital and post-discharge mortality. We conducted citation tracking for all eligible studies.
Méthode : Our search yielded 20,480 citations after removing duplicate records. We screened titles, abstracts and full-texts independently and in duplicate.
The prognosis research strategy group (PROGRESS) and the critical appraisal and data extraction for systematic review of prediction modelling studies (CHARMS) guidelines were followed. Study and outcome-specific risk of bias were assessed using the Quality in Prognosis Studies (QUIPS) instrument. We rated the certainty of evidence using the Grading of Recommendations, Assessment, Development and Evaluations (GRADE) recommendations for prognostic factor research.
Résultats : Four studies were included in this review and three were eligible for statistical pooling. Our sample comprised 1,134 persons who experienced in-hospital cardiac arrest (IHCA). The mean age of the sample was 71 years. The study results were pooled according to the specific frailty instrument. Three studies used the Clinical Frailty Scale (CFS) and adjusted age (our minimum confounder); the presence of frailty was associated with an approximate three-fold increase in the odds of dying in-hospital after IHCA (aOR = 2.93; 95% CI = 2.43-3.53, high certainty). Frailty was also associated with decreased incidence of ROSC (return of spontaneous circulation) and discharge home following IHCA. One study with high risk of bias used the Hospital Frailty Risk Score and reported a 43% decrease in the odds of discharge home for patients with frailty following IHCA.
Conclusion : High certainty evidence was found for an association between frailty and in-hospital mortality following IHCA. Frailty is a robust prognostic factor that contributes valuable information and can inform shared-decision making and policies surrounding advance care directives. Registration: PROSPERO Registration # CRD42020212922.
Conclusion (proposition de traduction) : Des preuves de haute certitude ont été trouvées pour une association entre la fragilité et la mortalité à l'hôpital après un arrêt cardiaque intra-hospitalier. La fragilité est un facteur pronostique solide qui fournit des informations précieuses et peut éclairer la prise de décision partagée et les politiques entourant les directives préalables en matière de soins.
Commentaire : La Société française de gériatrie et de gérontologie (SFGG) a adopté en 2011 la définition suivante de la fragilité :
« La fragilité est un syndrome clinique. Il reflète une diminution des capacités physiologiques de réserve qui altère les mécanismes d’adaptation au stress. Son expression clinique est modulée par les comorbidités et des facteurs psychologiques, sociaux, économiques et comportementaux. Le syndrome de fragilité est un marqueur de risque de mortalité et d’événements péjoratifs, notamment d’incapacités, de chutes, d’hospitalisation et d’entrée en institution. L’âge est un déterminant majeur de fragilité mais n’explique pas à lui seul ce syndrome. La prise en charge des déterminants de la fragilité peut réduire ou retarder ses conséquences. Ainsi, la fragilité s’inscrirait dans un processus potentiellement réversible » (Rolland 2011).
Deux modèles de critères de fragilité sont validés.
• Un modèle fondé sur un phénotype « physique » qui évalue la présence chez les personnes d’un âge ≥ 65 ans de 5 critères : perte de poids involontaire de plus de 4,5 kg (ou ≥ 5 % du poids) depuis 1 an, épuisement ressenti par le patient, vitesse de marche ralentie, baisse de la force musculaire et sédentarité. Les patients sont dits fragiles en présence de 3 critères ou plus. Ils sont dits « pré-fragiles » si au moins un des critères est présent. Si aucun des critères n’est présent ils sont considérés comme robustes (Fried 2001).
• Un autre modèle de fragilité prend en compte des critères fondés sur l’intégration de facteurs cognitifs et sociaux, regroupés sous le terme de « fragilité multi-domaine » intégrant : cognition, humeur, motivation, motricité, équilibre, capacités pour les activités de la vie quotidienne, nutrition, condition sociale et comorbidités (Rockwood 2005).
HAS Juin 2013. Comment repérer la fragilité en soins ambulatoires ? .
Cost-effectiveness of the i-gel supraglottic airway device compared to tracheal intubation during out-of-hospital cardiac arrest: Findings from the AIRWAYS-2 randomised controlled trial.
Stokes EA, Lazaroo MJ, Clout M, Brett SJ, Black S, Kirby K, Nolan JP, Reeves BC, Robinson M, Rogers CA, Scott LJ, Smartt H, South A, Taylor J, Thomas M, Voss S, Benger JR, Wordsworth S. | Resuscitation. 2021 Oct;167:1-9
DOI: https://doi.org/10.1016/j.resuscitation.2021.06.002
| Télécharger l'article au format
Keywords: Airway management; Cost-effectiveness analysis; Out of hospital cardiac arrest.
Clinical paper
Introduction : Optimal airway management during out-of-hospital cardiac arrest (OHCA) is uncertain. Complications from tracheal intubation (TI) may be avoided with supraglottic airway (SGA) devices. The AIRWAYS-2 cluster randomised controlled trial (ISRCTN08256118) compared the i-gel SGA with TI as the initial advanced airway management (AAM) strategy by paramedics treating adults with non-traumatic OHCA. This paper reports the trial cost-effectiveness analysis.
Méthode : A within-trial cost-effectiveness analysis of the i-gel compared with TI was conducted, with a six-month time horizon, from the perspective of the UK National Health Service (NHS) and personal social services. The primary outcome measure was quality-adjusted life years (QALYs), estimated using the EQ-5D-5L questionnaire. Multilevel linear regression modelling was used to account for clustering by paramedic when combining costs and outcomes.
Résultats : 9296 eligible patients were attended by 1382 trial paramedics and enrolled in the AIRWAYS-2 trial (4410 TI, 4886 i-gel). Mean QALYs to six months were 0.03 in both groups (i-gel minus TI difference -0.0015, 95% CI -0.0059 to 0.0028). Total costs per participant up to six months post-OHCA were £3570 and £3413 in the i-gel and TI groups respectively (mean difference £157, 95% CI -£270 to £583). Based on mean difference point estimates, TI was more effective and less costly than i-gel; however differences were small and there was great uncertainty around these results.
Conclusion : The small differences between groups in QALYs and costs shows no difference in the cost-effectiveness of the i-gel and TI when used as the initial AAM strategy in adults with non-traumatic OHCA.
Conclusion (proposition de traduction) : Les petites différences entre les groupes en termes d'années de vie ajustées sur la qualité et de coûts ne montrent aucune différence dans le rapport coût-efficacité de l'i-gel et de l'intubation trachéale lorsqu'ils sont utilisés comme stratégie initiale de gestion avancée des voies respiratoires chez l'adulte en arrêt cardiaque non traumatique en dehors de l'hôpital.
Physician's presence in pre-hospital setting improves one-month favorable neurological survival after out-of-hospital cardiac arrest: A propensity score matching analysis of the JAAM-OHCA Registry.
Hatakeyama T, Kiguchi T, Sera T, Nachi S, Ochiai K, Kitamura T, Ogura S, Otomo Y, Iwami T. | Resuscitation. 2021 Oct;167:38-46
DOI: https://doi.org/10.1016/j.resuscitation.2021.08.010
Keywords: Cardiac arrest; Cardiopulmonary resuscitation; Emergency medical services; Outcome; Resuscitation.
Clinical paper
Introduction : Using the out-of-hospital cardiac arrest (OHCA) registry in Japan, we evaluated the effectiveness of physicians' presence in pre-hospital settings after adjusting in-hospital treatments.
Méthode : This was a multicenter cohort study. We registered all consecutive OHCA patients in Japan who, from 1 June 2014 through 31 December 2017, were transported to institutions participating in the Japanese Association for Acute Medicine OHCA registry. We included OHCA patients aged at least 18 years, with medical etiology, and who received resuscitation from emergency medical services (EMS) personnel and medical professionals in hospitals. The primary outcome was one-month favorable neurological survival. We estimated the propensity score by fitting a logistic regression model that was adjusted for several variables before the arrival of EMS personnel and/or pre-hospital physician. A multivariable logistic regression analysis in propensity score-matched patients was used to adjust confounders, including extracorporeal membrane oxygenation, percutaneous coronary intervention, intra-aortic balloon pumping, and targeted temperature management.
Résultats : We analyzed 19,247 patients. Among them, 5.4% (N = 1040) had a neurologically favorable outcome. The adjusted odds ratio (AOR) of the physicians' presence compared with their absence for primary outcome was 1.84 (95% confidence interval (CI): 1.43-2.37). Among first documented non-shockable cardiac rhythm, the AOR was 1.51 (95% CI: 1.04-2.22). Among first documented shockable cardiac rhythm, the AOR of the physicians' presence for primary outcome was 1.15 (95% CI: 0.83-1.59).
Conclusion : The improved one-month favorable neurological survival was significantly associated with the physicians' presence in pre-hospital settings, compared with the physicians' absence.
Conclusion (proposition de traduction) : L'amélioration de la survie neurologique favorable à un mois était significativement associée à la présence des médecins en milieu préhospitalier, par rapport à l'absence des médecins.
The association of intraosseous vascular access and survival among pediatric patients with out-of-hospital cardiac arrest.
Besserer F, Kawano T, Dirk J, Meckler G, Tijssen JA, DeCaen A, Scheuermeyer F, Beno S, Christenson J, Grunau B; Canadian Resuscitation Outcomes Consortium. | Resuscitation. 2021 Oct;167:49-57
DOI: https://doi.org/10.1016/j.resuscitation.2021.08.005
Keywords: Cardiac arrest; Emergency medical services; Intraosseous; Pediatric; Vascular access.
Clinical paper
Introduction : In pediatric out-of-hospital cardiac arrest (OHCA) the effect of intraosseous (IO) or intravenous (IV) access on outcomes is unclear.
Méthode : We analyzed prospectively collected data of non-traumatic OHCA in the Resuscitation Outcomes Consortium registry from 2011 to 2015. We included EMS-treated patients ≤17 years of age, classified patients based on vascular access routes, and calculated success rates of IO and IV attempts. After excluding patients with obvious non-cardiac etiologies and those with unsuccessful vascular access or multiple routes, we fit a logistic regression model to evaluate the association of IO vascular access (reference IV access) with the primary outcome of survival, using multiple imputation to address missing data. We analyzed a subgroup of patients at least 2 years of age.
Résultats : There were 1549 non-traumatic OHCA: 895 (57.8%) patients had an IO line attempted with 822 (91.8%) successful; 488 (31.5%) had an IV line attempted with 345 (70.7%) successful (difference 21%, 95% CI 17 to 26%). Of the 761 patients included in our logistic regression, 601 received IO (30 [5.2%] survived) and 160 received IV (40 [25%] survived) vascular access. Intraosseous access was associated with a decreased probability of survival (adjusted OR 0.46; 95% CI 0.21-0.98). Patients at least 2 years of age showed a similar association (adjusted OR 0.36; CI 0.15-0.86).
Conclusion : Intraosseous access was associated with decreased survival among pediatric non-traumatic OHCA. These results are exploratory and support the need for further study to evaluate the effect of intravascular access method on outcomes.
Conclusion (proposition de traduction) : L'accès intra-osseux était associé à une diminution de la survie parmi les arrêts cardiaques pédiatriques non traumatiques extra-hospitaliers. Ces résultats sont exploratoires et appuient la nécessité d'une étude plus approfondie pour évaluer l'effet de la méthode d'accès intravasculaire sur les résultats.
Hypothermic Cardiac Arrest - Retrospective cohort study from the International Hypothermia Registry.
Walpoth BH, Maeder MB, Courvoisier DS, Meyer M, Cools E, Darocha T, Blancher M, Champly F, Mantovani L, Lovis C, Mair P. | Resuscitation. 2021 Oct;167:58-65
DOI: https://doi.org/10.1016/j.resuscitation.2021.08.016
| Télécharger l'article au format
Keywords: Accidental; Cardiac Arrest; ECLS; Hypothermia; Registry; Rewarming.
Clinical paper
Introduction : The International Hypothermia Registry (IHR) was created to increase knowledge of accidental hypothermia, particularly to develop evidence-based guidelines and find reliable outcome predictors. The present study compares hypothermic patients with and without cardiac arrest included in the IHR.
Méthode : Demographic, pre-hospital and in-hospital data, method of rewarming and outcome data were collected anonymously in the IHR between 2010 and 2020.
Résultats : Two hundred and one non-consecutive cases were included. The major causeof hypothermia was mountain accidents, predominantly in young men. Hypothermic Cardiac Arrest (HCA) occurred in 73 of 201 patients. Core temperature was significantly lower in the patients in cardiac arrest (25.0 vs. 30.0 °C, p < 0.001). One hundred and fifteen patients were rewarmed externally (93% with ROSC), 53 by extra-corporeal life support (ECLS) (40% with ROSC) and 21 with invasive internal techniques (71% with ROSC). The overall survival rate was 95% for patients with preserved circulation and 36% for those in cardiac arrest. Witnessed cardiac arrest and ROSC before rewarming were positive outcome predictors, asphyxia, coagulopathy, high potassium and lactate negative outcome predictors.
Conclusion : This first analysis of 201 IHR patients with moderate to severe accidental hypothermia shows an excellent 95% survival rate for patients with preserved circulation and 36% for HCA patients. Witnessed cardiac arrest, restoration of spontaneous circulation, low potassium and lactate and absence of asphyxia were positive survival predictors despite hypothermia in young, healthy adults after mountaineering accidents. However, accidental hypothermia is a heterogenous entity that should be considered in both treatment strategies and prognostication.
Conclusion (proposition de traduction) : Cette première analyse de 201 patients du Registre international d'hypothermie souffrant d'hypothermie accidentelle modérée à sévère montre un excellent taux de survie de 95 % pour les patients à circulation préservée et de 36 % pour les patients en arrêt cardiaque du à l'hypothermie. L'arrêt cardiaque observé, la restauration de la circulation spontanée, un faible taux de potassium et de lactate et l'absence d'asphyxie étaient des prédicteurs positifs de survie malgré l'hypothermie chez de jeunes adultes en bonne santé après des accidents d'alpinisme. Cependant, l'hypothermie accidentelle est une entité hétérogène qui doit être considérée à la fois dans les stratégies thérapeutiques et dans le pronostic.
Influence of sex on survival, neurologic outcomes, and neurodiagnostic testing after out-of-hospital cardiac arrest.
Vogelsong MA, May T, Agarwal S, Cronberg T, Dankiewicz J, Dupont A, Friberg H, Hand R, McPherson J, Mlynash M, Mooney M, Nielsen N, O'Riordan A, Patel N, Riker RR, Seder DB, Soreide E, Stammet P, Xiong W, Hirsch KG. | Resuscitation. 2021 Oct;167:66-75
DOI: https://doi.org/10.1016/j.resuscitation.2021.07.037
Keywords: Cardiac arrest; Gender; Neurodiagnostic testing; Outcomes; Sex; Withdrawal.
Clinical paper
Introduction : Previous studies evaluating the relationship between sex and post-resuscitation care and outcomes following out-of-hospital cardiac arrest (OHCA) are conflicting. We investigated the association between sex and outcomes as well as neurodiagnostic testing in a prospective multicenter international registry of patients admitted to intensive care units following OHCA.
Méthode : OHCA survivors enrolled in the International Cardiac Arrest Registry (INTCAR) from 2012 to 2017 were included. We assessed the independent association between sex and survival to hospital discharge, good neurologic outcome (Cerebral Performance Category 1 or 2), neurodiagnostic testing, and withdrawal of life-sustaining therapy (WLST).
Résultats : Of 2407 eligible patients, 809 (33.6%) were women. Baseline characteristics differed by sex, with less bystander CPR and initial shockable rhythms among women. Women were less likely to survive to hospital discharge, however significance abated following adjusted analysis (30.1% vs 42.7%, adjusted OR 0.85, 95% CI 0.67-1.08). Women were less likely to have good neurologic outcome at discharge (21.4% vs 34.0%, adjusted OR 0.74, 95% CI 0.57-0.96) and at six months post-arrest (16.7% vs 29.4%, adjusted OR 0.73, 95% CI 0.54-0.98) that persisted after adjustment. Neuroimaging (75.5% vs 74.3%, p = 0.54) and other neurophysiologic testing (78.8% vs 78.6%, p = 0.91) was similar across sex. Women were more likely to undergo WLST (55.6% vs 42.8%, adjusted OR 1.35, 95% CI 1.09-1.66).
Conclusion : Women with cardiac arrest have lower odds of good neurologic outcomes and higher odds of WLST, despite comparable rates of neurodiagnostic testing and after controlling for baseline differences in clinical characteristics and cardiac arrest features.
Conclusion (proposition de traduction) : Les femmes victimes d'un arrêt cardiaque ont une probabilité plus faible d'obtenir de bons résultats neurologiques et une probabilité plus élevée d'arrêt du traitement de maintien de la vie, malgré des taux comparables de tests neurodiagnostiques et après contrôle des différences de base dans les caractéristiques cliniques et les caractéristiques de l'arrêt cardiaque.
The association between end-tidal CO2 and return of spontaneous circulation after out-of-hospital cardiac arrest with pulseless electrical activity.
Crickmer M, Drennan IR, Turner L, Cheskes S. | Resuscitation. 2021 Oct;167:76-81
DOI: https://doi.org/10.1016/j.resuscitation.2021.08.014
Keywords: Cardiac arrest; ETCO2; Emergency medical services; Pulseless electrical activity; Resuscitation; Return of spontaneous circulation.
Clinical paper
Introduction : End-tidal carbon dioxide (ETCO2) has been suggested to have prognostic implications during out-of-hospital cardiac arrest (OHCA). Our objective was to determine if the change in ETCO2 (delta ETCO2) during resuscitation was predictive of future return of spontaneous circulation (ROSC) in patients with pulseless electrical activity (PEA) arrests.
Méthode : We performed a retrospective, observational study of adult (≥18 years of age) non-traumatic PEA OHCAs in two Canadian EMS systems over a two-year time frame beginning on January 1, 2018. Cases were excluded if there was a Do Not Resuscitate order (DNR), had no advanced airway, or had less than two ETCO2 recordings. We performed multivariable logistic regression to examine the association between ETCO2 measures and ROSC. Second, we examined the prognostic performance (sensitivity, specificity, NPV, PPV) for ETCO2 at specific thresholds for predicting ROSC.
Résultats : A total of 208 OHCA met inclusion criteria of which 67 (32%) obtained ROSC. After adjusting for pre-determined confounders, there was an association between delta ETCO2 and ROSC (odds ratio [OR] per 10 mmHg increase in ETCO2 of 1.74 (95% confidence interval [CI] 1.35 to 2.24); P value < 0.001). We also found significant associations between both initial ETCO2 and final ETCO2 with ROSC.
Conclusion : Our analysis indicates that there is a positive linear relationship between delta ETCO2 and ROSC with values of delta ETCO2 > 20 mmHg being highly specific for ROSC in PEA patients. As such, patients with up-trending ETCO2 values should have resuscitation continued unless there is overwhelming clinical evidence to the contrary.
Conclusion (proposition de traduction) : Notre analyse indique qu'il existe une relation linéaire positive entre la modification du taux d'EtCO2 et le RACS avec des valeurs de modification du taux d'EtCO2 > 20 mmHg étant hautement spécifiques pour la RACS chez les patients en arrêt cardiaque avec activité électrique sans pouls. En tant que tels, les patients dont les valeurs d'EtCO2 tendent à augmenter devraient continuer à être réanimer, à moins qu'il n'y ait des preuves cliniques écrasantes du contraire.
Is point-of-care ultrasound a reliable predictor of outcome during traumatic cardiac arrest? A systematic review and meta-analysis from the SHoC investigators.
Lalande E, Burwash-Brennan T, Burns K, Harris T, Thomas S, Woo MY, Atkinson P. | Resuscitation. 2021 Oct;167:128-136
DOI: https://doi.org/10.1016/j.resuscitation.2021.08.027
Keywords: Point-of-care ultrasound; Prognosis; Traumatic arrest.
Clinical paper
Introduction : Point-of-care ultrasound (POCUS) has been shown to assist in predicting outcomes in cardiac arrest. We evaluated the test characteristics of POCUS in predicting poor outcomes: failure of return of spontaneous circulation (ROSC), survival to hospital admission (SHA), survival to hospital discharge (SHD) and neurologically intact survival to hospital discharge (NISHD) in adult and paediatric patients with blunt and penetrating traumatic cardiac arrest (TCA) in out-of-hospital or emergency department settings.
Méthode : We conducted a systematic review and meta-analysis using the PRISMA guidelines. We searched Clinicaltrials.gov, CINAHL, Cochrane library, EMBASE, Medline and the World Health Organization-International Clinical Trials Registry from 1974 to November 9, 2020. Risk of bias was assessed using QUADAS-2 tool. We used a random-effects meta-analysis model with 95% confidence intervals with I2 statistics for heterogeneity.
Résultats : We included 8 studies involving 710 cases of TCA. For all blunt and penetrating TCA patients who failed to achieve ROSC, the specificity (proportion of patients with cardiac activity on POCUS who achieved ROSC) was 98% (95% CI 0.13 to 1.0). The sensitivity (proportion of patients with cardiac standstill on POCUS who failed to achieve ROSC) was 91% (95% CI 0.67 to 0.98). No patient with cardiac standstill survived. Substantial level of heterogeneity was noted.
Conclusion : Patients in TCA without cardiac activity on POCUS have a high likelihood of death and negligible chance of SHD. The numbers of patients included in published studies remains too low for practice recommendations for termination of resuscitation based solely upon the absence of cardiac activity on POCUS.
Conclusion (proposition de traduction) : Les patients retrouvé en arrêt cardiaque traumatique sans activité cardiaque à l'échographie au point d'intervention ont une probabilité élevée de décès et une chance négligeable de survie jusqu'à la sortie de l'hôpital. Le nombre de patients inclus dans les études publiées reste trop faible pour des recommandations de pratique pour l'arrêt de la réanimation basées uniquement sur l'absence d'activité cardiaque à l'échographie au point d'intervention.
Incidence of cardiac interventions and associated cardiac arrest outcomes in patients with nonshockable initial rhythms and no ST elevation post resuscitation.
Harhash AA, May T, Hsu CH, Seder DB, Dankiewicz J, Agarwal S, Patel N, McPherson J, Riker R, Soreide E, Hirsch KG, Stammet P, Dupont A, Forsberg S, Rubertsson S, Friberg H, Nielsen N, Mooney MR, Kern KB. | Resuscitation. 2021 Oct;167:188-197
DOI: https://doi.org/10.1016/j.resuscitation.2021.08.026
Keywords: Cardiac arrest; Coronary angiography; NSTEMI; Neurological recovery; Nonshockable rhythm; Outcomes.
Clinical paper
Introduction : Out of Hospital Cardiac arrest (OHCA) survivors with ST elevation (STE) with or without shockable rhythms often benefit from coronary angiography (CAG) and, if indicated, percutaneous coronary intervention (PCI). However, the benefits of CAG and PCI in OHCA survivors with nonshockable rhythms (PEA/asystole) and no STE are debated.
Méthode : Using the International Cardiac Arrest Registry (INTCAR 2.0), representing 44 centers in the US and Europe, comatose OHCA survivors with known presenting rhythms and post resuscitation ECGs were identified. Survival to hospital discharge, neurological recovery on discharge, and impact of CAG with or without PCI on such outcome were assessed and compared with other groups (shockable rhythms with or without STE).
Résultats : Total of 2113 OHCA survivors were identified and described as; nonshockable/no STE (Nsh-NST) (n = 940, 44.5%), shockable/no STE (Sh-NST) (n = 716, 33.9%), nonshockable/STE (Nsh-ST) (n = 110, 5.2%), and shockable/STE (Sh-ST) (n = 347, 16.4%). Of Nsh-NST, 13.7% (129) were previously healthy before CA and only 17.3% (161) underwent CAG; of those, 30.4% (52) underwent PCI. A total of 18.6% (174) Nsh-NST patients survived to hospital discharge, with 57.5% (100) of such survivors having good neurological recovery (cerebral performance category 1 or 2) on discharge. Coronary angiography was associated with improved odds for survival and neurological recovery among all groups, including those with NSh-NST.
Conclusion : Nonshockable initial rhythms with no ST elevation post resuscitation was the most common presentation after OHCA. Although most of these patients did not undergo coronary angiography, among those who did, 1 in 4 patients had a culprit lesion and underwent revascularization. Invasive CAG should be at least considered for all OHCA survivors, including those with nonshockable rhythms and no ST elevation post resuscitation.
Conclusion (proposition de traduction) : Les rythmes initiaux non choquants sans élévation du segment ST après réanimation étaient la présentation la plus courante après un arrêt cardiaque en dehors de l'hôpital. Bien que la plupart de ces patients n'aient pas bénéficié d'une angiographie coronaire, parmi ceux qui l'ont fait, 1 patient sur 4 avait une lésion responsable et a bénéficié d'une revascularisation. Une coronarographie invasive doit être envisagée au moins pour tous les survivants d'un arrêt cardiaque en dehors de l'hôpital, y compris ceux qui présentent des rythmes non choquables et sans élévation du segment ST après réanimation.
Accessibility of automatic external defibrillators and survival rate of people with out-of-hospital cardiac arrest: A systematic review of real-world studies.
Ruan Y, Sun G, Li C, An Y, Yue L, Zhu M, Liu Y, Zou K, Chen D. | Resuscitation. 2021 Oct;167:200-208
DOI: https://doi.org/10.1016/j.resuscitation.2021.08.035
Keywords: Accessibility; Automatic external defibrillators; Out-of-hospital cardiac arrest; Survival rate.
Clinical paper
Introduction : o evaluate the relationship between the accessibility of automatic external defibrillators (AEDs) and the survival rate of patients who have out-of-hospital cardiac arrest (OHCA).
Méthode : The systematic review was conducted according to the Cochrane Handbook of Systematic Reviews. We searched the Chinese and English literature databases from 2009 to 2019. Study selection and data collection were conducted by three reviewers. One-month survival rates of OHCA with different AEDs accessibility were estimated using meta-analysis.
Résultats : Overall 16 studies with 55,537 participants were included. The overall one-month survival rate for OHCA was 27.4%. The one-month survival rate was 35.2% for people receiving AEDs within 5 min, 36.6% between 5 min to 10 min, and 28.4% for longer than 10 min. By distance between the location of the AEDs and the location of the cardiac arrest, the one-month survival rate was 37.1% for those ≤100 m, 22.0% for 100 m-200 m, and 12.8% for >200 m, respectively. The one-month survival rate was 39.3% in schools, sports venues and airports compared with 23.5% in other sites. The number of AEDs allocation was positively correlated, while the time and distance were negatively correlated with the one-month survival rate adjusted for other factors, but they were all non-significant correlations.
Conclusion : The improvement of accessibility of AEDs may increase the survival rate of OHCA and the survival rate may be higher in playgrounds, airports, and schools equipped with AEDs. However, the strength of evidence was limited by the considerably heterogeneity of included studies. Verification of these findings in further studies is warranted.
Conclusion (proposition de traduction) : L'amélioration de l'accessibilité des DAE peut augmenter le taux de survie de l'arrêt cardiaque en dehors de l'hôpital et le taux de survie peut être plus élevé dans les terrains de jeux, les aéroports et les écoles équipées de DAE. Cependant, la force des preuves était limitée par l'hétérogénéité considérable des études incluses. La vérification de ces résultats dans d'autres études est justifiée.
Prehospital Tibial Intraosseous Drug Administration is Associated with Reduced Survival Following Out of Hospital Cardiac Arrest: A study for the CARES Surveillance Group.
Hamam MS, Klausner HA, France J, Tang A, Swor RA, Paxton JH, O'Neil BJ, Brent C, Neumar RW, Dunne RB, Reddi S, Miller J. | Resuscitation. 2021 Oct;167:261-266
DOI: https://doi.org/10.1016/j.resuscitation.2021.06.016
Keywords: Cardiopulmonary resuscitation; Intraosseous drug administration; Out-of-hospital cardiac arrest.
Clinical paper
Introduction : Recent reports have questioned the efficacy of intraosseous (IO) drug administration for out-of-hospital cardiac arrest (OHCA) resuscitation. Our aim was to determine whether prehospital administration of resuscitative medications via the IO route was associated with lower rates of return of spontaneous circulation (ROSC) and survival to hospital discharge than peripheral intravenous (IV) infusion in the setting of OHCA.
Méthode : We obtained data on all OHCA patients receiving prehospital IV or IO drug administration from the three most populous counties in Michigan over three years. Data was from the Michigan Cardiac Arrest Registry to Enhance Survival (CARES) database. The association between route of drug administration and outcomes was tested using a matched propensity score analysis.
Résultats : From a total of 10,626 OHCA patients, 6869 received parenteral drugs during their prehospital resuscitation (37.8% by IO) and were included in analysis. Unadjusted outcomes were lower in patients with IO vs. IV access: 18.3% vs. 23.8% for ROSC (p < 0.001), 3.2% vs. 7.6% for survival to hospital discharge (p < 0.001), and 2.0% vs. 5.8% for favorable neurological function (p < 0.001). After adjustment, IO route remained associated with lower odds of sustained ROSC (OR 0.72, 95% CI 0.63-0.81, p < 0.001), hospital survival (OR 0.48, 95% CI 0.37-0.62, p < 0.001), and favorable neurological outcomes (OR 0.42, 95% CI 0.30-0.57, p < 0.001).
Conclusion : In this cohort of OHCA patients, the use of prehospital IO drug administration was associated with unfavorable clinical outcomes.
Conclusion (proposition de traduction) : Dans cette cohorte de patients en arrêt cardiaque extra-hospitalier, l'utilisation de l'administration intra-osseuse préhospitalière de médicaments était associée à des résultats cliniques défavorables.
Fewer tracheal intubation attempts are associated with improved neurologically intact survival following out-of-hospital cardiac arrest.
Murphy DL, Murphy DL, Bulger NE, Harrington BM, Skerchak JA, Counts CR, Latimer AJ, Yang BY, Maynard C, Rea TD, Sayre MR. | Resuscitation. 2021 Oct;167:289-296
DOI: https://doi.org/10.1016/j.resuscitation.2021.07.001
| Télécharger l'article au format
Keywords: Airway management; Cardiopulmonary resuscitation; Emergency medical services; Emergency medical technicians; Heart arrest; Intratracheal; Intubation.
Clinical paper
Introduction : International guidelines emphasize advanced airway management during out-of-hospital cardiac arrest (OHCA). We hypothesized that increasing endotracheal intubation attempts during OHCA were associated with a lower likelihood of favorable neurologic survival at discharge.
Méthode : This retrospective, observational cohort evaluated the relationship between number of intubation attempts and favorable neurologic survival among non-traumatic OHCA patients receiving cardiopulmonary resuscitation (CPR) from January 1, 2015-June 30, 2019 in a large urban emergency medical services (EMS) system. Favorable neurologic status at hospital discharge was defined as a Cerebral Performance Category score of 1 or 2. Multivariable logistic regression, adjusted for age, sex, witness status, bystander CPR, initial rhythm, and time of EMS arrival, was performed using the number of attempts as a continuous variable.
Résultats : Over 54 months, 1205 patients were included. Intubation attempts per case were 1 = 757(63%), 2 = 279(23%), 3 = 116(10%), ≥4 = 49(4%), and missing/unknown in 4(<1%). The mean (SD) time interval from paramedic arrival to intubation increased with the number of attempts: 1 = 4.9(2.4) min, 2 = 8.0(2.9) min, 3 = 10.9(3.3) min, and ≥4 = 15.5(4.4) min. Final advanced airway techniques employed were endotracheal intubation (97%), supraglottic devices (3%), and cricothyrotomy (<1%). Favorable neurologic outcome declined with each additional attempt: 11% with 1 attempt, 4% with 2 attempts, 3% with 3 attempts, and 2% with 4 or more attempts (AOR = 0.41, 95% CI 0.25-0.68).
Conclusion : ncreasing number of intubation attempts during OHCA resuscitation was associated with lower likelihood of favorable neurologic outcome.
Conclusion (proposition de traduction) : Le nombre croissant de tentatives d'intubation pendant la réanimation d'un arrêt cardiaque en dehors de l'hôpital était associé à une probabilité plus faible de résultats neurologiques favorables.
Neurological outcome in adult out-of-hospital cardiac arrest - Not all doom and gloom!.
Mckenzie N, Ball S, Bailey P, Finn L, Arendts G, Celenza A, Fatovich D, Jenkins I, Mukherjee A, Smedley B, Ghedina N, Bray J, Ho KM, Dobb G, Finn J. | Resuscitation. 2021 Oct;167:227-232
DOI: https://doi.org/10.1016/j.resuscitation.2021.08.042
Keywords: Cerebral performance category; Neurological outcome; Out-of-hospital cardiac arrest; Overall performance category; Survival.
Short Paper
Introduction : To describe neurological and functional outcomes among out-of-hospital cardiac arrest (OHCA) patients who survived to hospital discharge; to determine the association between neurological outcome at hospital discharge and 12-month survival.
Méthode : Our cohort comprised adult OHCA patients (≥18 years) attended by St John WA (SJWA) paramedics in Perth, Western Australia (WA), who survived to hospital discharge, between 1st January 2004 and 31st December 2019. Neurological and functional status at hospital discharge (and before the arrest) was determined by medical record review using the five-point 'Cerebral Performance Category (CPC)' and 'Overall Performance Category (OPC)' scores. Adjusted multivariable logistic regression analysis was used to estimate the association of CPC score at hospital discharge with 12-month survival, adjusted for prognostic variables.
Résultats : Over the study period, SJWA attended 23,712 OHCAs. Resuscitation was attempted in 43.4% of cases (n = 10,299) with 2171 subsequent admissions, 99.4% (n = 2158) of these were admitted to a study hospital. Of the 1062 hospital survivors, 71.3% (n = 757) were CPC1 (highest category of neurological performance), 21.4% (n = 227) CPC2, 6.3% (n = 67) CPC3 and 1.0% (n = 11) CPC4. OPC scores followed a similar distribution. Of the 1,011 WA residents who survived to hospital discharge, 92.3% (n = 933) survived to 12-months. A CPC1-2 at hospital discharge was significantly associated with 12-month survival (adjusted odds ratio 3.28, 95% confidence interval 1.69-6.39).
Conclusion : Whilst overall survival is low, most survivors of OHCA have a good neurological outcome at hospital discharge and are alive at 12-months.
Conclusion (proposition de traduction) : Alors que la survie globale est faible, la plupart des survivants d'un arrêt cardiaque en dehors de l'hôpital ont un bon pronostic neurologique à la sortie de l'hôpital et sont vivants à 12 mois.
Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine
The development of emergency medical services benefit score: a European Delphi study.
Heino A, Raatiniemi L, Iirola T, Meriläinen M, Liisanantti J, Tommila M; Collaboration Group. | Scand J Trauma Resusc Emerg Med. 2021 Oct 16;29(1):151
DOI: https://doi.org/10.1186/s13049-021-00966-3
| Télécharger l'article au format
Keywords: Delphi method; Emergency medical services; Prehospital; Quality control.
Original research
Introduction : The helicopter emergency services (HEMS) Benefit Score (HBS) is a nine-level scoring system developed to evaluate the benefits of HEMS missions. The HBS has been in clinical use for two decades in its original form. Advances in prehospital care, however, have produced demand for a revision of the HBS. Therefore, we developed the emergency medical services (EMS) Benefit Score (EBS) based on the former HBS. As reflected by its name, the aim of the EBS is to measure the benefits produced by the whole EMS systems to patients.
Méthode : This is a four-round, web-based, international Delphi consensus study with a consensus definition made by experts from seven countries. Participants reviewed items of the revised HBS on a 5-point Likert scale. A content validity index (CVI) was calculated, and agreement was defined as a 70% CVI. Study included experts from seven European countries. Of these, 18 were prehospital expert panellists and 11 were in-hospital commentary board members.
Résultats : The first Delphi round resulted in 1248 intervention examples divided into ten diagnostic categories. After removing overlapping examples, 413 interventions were included in the second Delphi round, which resulted in 38 examples divided into HBS categories 3-8. In the third Delphi round, these resulted in 37 prehospital interventions, examples of which were given revised version of the score. In the fourth and final Delphi round, the expert panel was given an opportunity to accept or comment on the revised scoring system.
Conclusion : The former HBS was revised by a Delphi methodology and EBS developed to represent its structural purpose better. The EBS includes 37 exemplar prehospital interventions to guide its clinical use.
Conclusion (proposition de traduction) : L’ancien score des services d’urgence pour les hélicoptères a été révisé par une méthodologie Delphi et le score des services d’urgence pour les hélicoptères a été élaboré pour mieux représenter son objectif structurel. Le Benefit Score des services d’urgence par hélicoptère comprend 37 interventions préhospitalières exemplaires pour guider son utilisation clinique.
Shock
Evaluation of Evidence, Pharmacology, and Interplay of Fluid Resuscitation and Vasoactive Therapy in Sepsis and Septic Shock.
Barlow B, Bissell BD. | Shock. 2021 Oct 1;56(4):484-492
DOI: https://doi.org/10.1097/shk.0000000000001783
Keywords: Aucun
Review Article
Editorial : We sought to review the pharmacology of vasoactive therapy and fluid administration in sepsis and septic shock, with specific insight into the physiologic interplay of these agents. A PubMed/MEDLINE search was conducted using the following terms (vasopressor OR vasoactive OR inotrope) AND (crystalloid OR colloid OR fluid) AND (sepsis) AND (shock OR septic shock) from 1965 to October 2020. A total of 1,022 citations were reviewed with only relevant clinical data extracted. While physiologic rationale provides a hypothetical foundation for interaction between fluid and vasopressor administration, few studies have sought to evaluate the clinical impact of this synergy. Current guidelines are not in alignment with the data available, which suggests a potential benefit from low-dose fluid administration and early vasopressor exposure. Future data must account for the impact of both of these pharmacotherapies when assessing clinical outcomes and should assess personalization of therapy based on the possible interaction.
Conclusion : Minimal data are available to inform guideline recommendations for IVF resuscitation strategies, and ambiguity remains regarding timing of vasoactive initiation. Alternate recommendations have been forthcoming, but evidence is minimal. Physiologic rationale supports an interplay between resuscitation fluids and vasopressor exposure and observational studies demonstrate that early, intermediate IVF volumes (i.e., 1 L–2.5 L) followed by expedient vasopressor initiation are associated with the best predicted clinical outcomes. Randomized, controlled trials are needed to test this hypothesis as the guidelines continue to recommend aggressive fluid resuscitation with utilization of vasoactive therapy in patients with shock despite fluid resuscitation. Future studies must evaluate the impact of fluid exposure on vasopressor dosing and duration as well as the utilization of vasoactive therapies and influence on crystalloid requirement.
Conclusion (proposition de traduction) : Des données mineures sont disponibles pour éclairer les recommandations des lignes directrices sur la stratégies de remplissage vasculaire par voie intraveineuse, et l'ambiguïté demeure concernant le moment de l'initiation de l'introduction des catécholamines. D'autres recommandations ont été formulées, mais les preuves sont minimes. La justification physiologique soutient une interaction entre le remplissage vasculaire et l'exposition aux vasopresseurs et les études observationnelles démontrent que les volumes de fluides intraveineux précoces et intermédiaires (càd 1 L-2,5 L). Des essais contrôlés randomisés sont nécessaires pour tester cette hypothèse, car les lignes directrices continuent de recommander une remplissage vasculaire agressif avec utilisation d'un traitement vasoactif chez les patients en état de choc malgré la réanimation liquidienne. Les études futures doivent évaluer l'impact de l'exposition aux liquides sur le dosage et la durée des vasopresseurs ainsi que l'utilisation des thérapies vasoactives et l'influence sur les besoins en cristalloïdes.
Outcomes Associated With Norepinephrine Use Among Cardiac Intensive Care Unit Patients with Severe Shock.
Burstein B, Vallabhajosyula S, Ternus B, Murphree D, Barsness GW, Kashani K, Jentzer JC. | Shock. 2021 Oct 1;56(4):522-528
DOI: https://doi.org/10.1097/shk.0000000000001767
Keywords: Aucun
Clinical Science Aspect
Introduction : Recent data suggests improved outcomes among cardiac intensive care unit (CICU) patients treated with norepinephrine, especially patients with severe shock. We aimed to describe the association between norepinephrine and mortality in CICU patients with severe shock, defined as those requiring high-dose vasopressors (HDV).
Méthode : We retrospectively evaluated Mayo Clinic CICU patients treated with vasopressors from 2007 to 2015. HDV was defined as a peak Cumulative Vasopressor Index of four for any vasopressor. Peak norepinephrine equivalent (NEE) dose was used to compare vasopressor doses. Multivariable logistic regression was used to determine predictors of hospital mortality.
Résultats : We included 2,090 patients with a median age of 69 years (IQR 59-78), including 35% females; 44% of patients received HDV. Hospital mortality was higher among patients receiving HDV (42% vs. 16%, unadjusted OR 3.87, 95% CI 3.16-4.75, P < 0.01). On multivariable analysis in HDV patients, hospital mortality increased with rising peak NEE (adjusted OR 1.02 per 0.01 mcg/kg/min, 95% CI 1.01-1.02, P < 0.01) and the use of NE was associated with lower hospital mortality (adjusted OR 0.46, 95% CI 0.31-0.72, P < 0.01). After adjustment for illness severity, peak NEE and norepinephrine use were not associated with mortality among patients who did not require HDV.
Conclusion : Mortality is high among CICU patients requiring HDV, and rises with increasing vasopressor requirements. Use of NE was associated with lower mortality among patients requiring HDV, but not among those without HDV, implying that patients with more severe shock may benefit from preferential use of NE.
Conclusion (proposition de traduction) : La mortalité est élevée chez les patients des unités de soins intensifs cardiaques nécessitant des vasopresseurs à forte dose et augmente avec l'augmentation des besoins en vasopresseurs. L'utilisation de la noradrénaline était associée à une mortalité plus faible chez les patients nécessitant des vasopresseurs à forte dose, mais pas chez ceux sans vasopresseur à forte dose, ce qui implique que les patients présentant un choc plus sévère peuvent bénéficier d'une utilisation préférentielle de la noradrénaline.
Associations Between Elevated Systolic Blood Pressure and Outcomes in Critically Ill Patients: A Retrospective Cohort Study and Propensity Analysis.
Hu AM, Hai C, Wang HB, Zhang Z, Sun LB, Zhang ZJ, Li HP. | Shock. 2021 Oct 1;56(4):557-563
DOI: https://doi.org/10.1097/shk.0000000000001774
Keywords: Aucun
Clinical Science Aspect
Introduction : Studies have shown nonlinear relationships between systolic blood pressure (SBP) and outcomes, with increased risk observed at both low and high blood pressure levels. However, the relationships between cumulative times at different SBP levels and outcomes in critically ill patients remain unclear. We hypothesized that an appropriate SBP level is associated with a decrease in adverse outcomes after intensive care unit (ICU) admission.
Méthode : This study was a retrospective analysis of data from the Medical Information Mart for Intensive Care (MIMIC) III database, which includes more than 1,000,000 SBP records from 12,820 patients. Associations of cumulative times at four SBP ranges (<100 mm Hg, 100-120 mm Hg, 120-140 mm Hg, and ≥140 mm Hg) with mortality (12-, 3-, 1-month mortality and in-hospital mortality) were evaluated. Restricted cubic splines and multivariable Cox regression models were employed to assess associations between mortality and cumulative times at SBP levels (4 levels: <2, 2-12, 12-36, and ≥36 h) over 72 h of ICU admission. Additionally, 120 mm Hg to 140 mm Hg was subdivided into <12 h (Group L) and ≥12 h (Group M) subsets and subjected to propensity-score matching and subgroup analyses.
Résultats : At 120 mm Hg to 140 mm Hg, level-4 SBP was associated with lower adjusted risks of mortality at 12 months (OR, 0.71; CI, 0.61-0.81), 3 months (OR, 0.72; CI, 0.61-0.85), and 1 month (OR, 0.61; CI, 0.48-0.79) and in the hospital (OR, 0.71; CI, 0.58-0.88) than level-1 SBP. The cumulative times at the other 3 SBP ranges (<100 mm Hg, 100-120 mm Hg, and ≥140 mm Hg) were not independent risk predictors of prognosis. Furthermore, Group M had lower 12-month mortality than Group L, which remained in the propensity-score matched and subgroup analyses.
Conclusion : SBP at 120 mm Hg to 140 mm Hg was associated with decreased adverse outcomes. Randomized trials are required to determine whether the outcomes in critically ill patients improve with early maintenance of a SBP level at 120 mm Hg to 140 mm Hg.
Conclusion (proposition de traduction) : Une pression artérielle systolique de 120 mmHg à 140 mmHg était associée à une diminution des effets indésirables. Des essais randomisés sont nécessaires pour déterminer si les résultats chez les patients de réanimation s'améliorent avec le maintien précoce d'un niveau de pression artérielle systolique compris entre 120 mmHg à 140 mmHg.
Stroke
Thrombectomy in Extensive Stroke May Not Be Beneficial and Is Associated With Increased Risk for Hemorrhage.
Meyer L, Bechstein M, Bester M, Hanning U, Brekenfeld C, Flottmann F, Kniep H, van Horn N, Deb-Chatterji M, Thomalla G, Sporns P, Yeo LL, Tan BY, Gopinathan A, Kastrup A, Politi M, Papanagiotou P, Kemmling A, Fiehler J, Broocks G; German Stroke Registry–Endovascular Treatment (GSR-ET). | Stroke. 2021 Oct;52(10):3109-3117
DOI: https://doi.org/10.1161/strokeaha.120.033101
Keywords: Aucun
Original Contribution
Introduction : This study evaluates the benefit of endovascular treatment (EVT) for patients with extensive baseline stroke compared with best medical treatment.
Méthode : This retrospective, multicenter study compares EVT and best medical treatment for computed tomography (CT)–based selection of patients with extensive baseline infarcts (Alberta Stroke Program Early CT Score ≤5) attributed to anterior circulation stroke. Patients were selected from the German Stroke Registry and 3 tertiary stroke centers. Primary functional end points were rates of good (modified Rankin Scale score of ≤3) and very poor outcome (modified Rankin Scale score of ≥5) at 90 days. Secondary safety end point was the occurrence of symptomatic intracerebral hemorrhage. Angiographic outcome was evaluated with the modified Thrombolysis in Cerebral Infarction Scale.
Résultats : After 1:1 pair matching, a total of 248 patients were compared by treatment arm. Good functional outcome was observed in 27.4% in the EVT group, and in 25% in the best medical treatment group (P=0.665). Advanced age (adjusted odds ratio, 1.08 [95% CI, 1.05–1.10], P<0.001) and symptomatic intracerebral hemorrhage (adjusted odds ratio, 6.35 [95% CI, 2.08–19.35], P<0.001) were independently associated with very poor outcome. Mortality (43.5% versus 28.9%, P=0.025) and symptomatic intracerebral hemorrhage (16.1% versus 5.6%, P=0.008) were significantly higher in the EVT group. The lowest rates of good functional outcome (≈15%) were observed in groups of failed and partial recanalization (modified Thrombolysis in Cerebral Infarction Scale score of 0/1–2a), whereas patients with complete recanalization (modified Thrombolysis in Cerebral Infarction Scale score of 3) with recanalization attempts ≤2 benefitted the most (modified Rankin Scale score of ≤3:42.3%, P=0.074) compared with best medical treatment.
Conclusion : In daily clinical practice, EVT for CT–based selected patients with low Alberta Stroke Program Early CT Score anterior circulation stroke may not be beneficial and is associated with increased risk for hemorrhage and mortality, especially in the elderly. However, first- or second-pass complete recanalization seems to reveal a clinical benefit of EVT highlighting the vulnerability of the low Alberta Stroke Program Early CT Score subgroup.
Conclusion (proposition de traduction) : Dans la pratique clinique quotidienne, le traitement endovasculaire chez les patients sélectionnés par tomodensitométrie ayant un score Alberta Stroke Program Early CT faible lors d’un AVC de la circulation antérieure peut ne pas être bénéfique et être associée à un risque accru d’hémorragie et de mortalité, en particulier chez les personnes âgées. Cependant, la revascularisation complète au premier ou au deuxième passage semble révéler un avantage clinique du traitement endovasculaire mettant en évidence la vulnérabilité du sous-groupe de score Alberta Stroke Program Early CT faible.
The American Journal of Emergency Medicine
Topical ketamine as a local anesthetic agent in reducing venipuncture pain: A randomized controlled trial.
Heydari F, Khalilian S, Golshani K, Majidinejad S, Masoumi B, Massoumi A. | Am J Emerg Med. 2021 Oct;48:48-53
DOI: https://doi.org/10.1016/j.ajem.2021.03.055
Keywords: Emergency department; Ketamine; Lidocaine-prilocaine cream; Pain; Venipuncture.
Research article
Introduction : Pain control is an important aspect of ED patient management, and there are many different protocols used around the world influenced by both availability of local resources as well as staff competency and experience. This study aims to evaluate the use of topical ketamine in acute pain reduction by directly comparing it to lidocaine-prilocaine (EMLA) cream.
Méthode : In this randomized clinical trial, 300 adult patients classified as level 4 or 5 by ESI triage system were enrolled. These patients were divided randomly into three groups. The site of venipuncture was covered with 2 g of topical ketamine cream 10% in group one, 2 g of 5% EMLA cream in group two, and finally, in group 3 (control group), was covered with placebo (2 g of cold cream). The primary end point of the study was reported pain severity with secondary end points being onset of local anesthesia as well as any side effects noted.
Résultats : The data gathered showed pain score during venipuncture in both intervention groups were significantly lower when compared to the control group (P < 0.05). However, pain score did not differ between the 2 intervention groups (P = 0.395). There was no statistically significant difference between the ketamine or EMLA in onset of local anesthesia (P = 0.419). We noted itching and irritation was significantly higher in the EMLA group when compared to ketamine(P < 0.05).
Conclusion : This study showed that local cutaneous ketamine is as effective as EMLA in relieving pain during venipuncture.
Conclusion (proposition de traduction) : Cette étude a montré que la kétamine cutanée locale est aussi efficace que l'EMLA pour soulager la douleur lors de la ponction veineuse.
Continuous chest compressions with asynchronous ventilation improve survival in a neonatal swine model of asphyxial cardiac arrest.
Aggelina A, Pantazopoulos I, Giokas G, Chalkias A, Mavrovounis G, Papalois A, Douvanas A, Xanthos T, Iacovidou N. | Am J Emerg Med. 2021 Oct;48:60-66
DOI: https://doi.org/10.1016/j.ajem.2021.04.009
Keywords: Asphyxial cardiac arrest; Continuous chest compressions; Neonatal resuscitation; ROSC; Survival.
Research article
Introduction : Guidelines for neonatal resuscitation recommend a 3:1 compression to ventilation ratio. However, this recommendation is based on expert opinion and consensus rather than strong scientific evidence. Our primary aim was to assess whether continuous chest compressions with asynchronous ventilations would increase return of spontaneous circulation (ROSC) rate and survival compared to the 3:1 chest compression to ventilation ratio.
Méthode : This was a prospective, randomized, laboratory study. Twenty male Landrace-Large White pigs, aged 1-4 days with an average weight 1.650 ± 228.3 g were asphyxiated and left untreated until heart rate was less than 60 bpm or mean arterial pressure was below 15 mmHg. Animals were then randomly assigned to receive either continuous chest compressions with asynchronous ventilations (n = 10), or standard (3:1) chest compression to ventilation ratio (n = 10). Heart rate and arterial pressure were assessed every 30 s during cardiopulmonary resuscitation (CPR) until ROSC or asystole. All animals with ROSC were monitored for 4 h.
Résultats : Coronary perfusion pressure (CPP) at 30 s of CPR was significantly higher in the experimental group (45.7 ± 16.9 vs. 21.8 ± 6 mmHg, p < 0.001) and remained significantly elevated throughout the experiment. End-tidal carbon dioxide (ETCO2) was also significantly higher in the experimental group throughout the experiment (23.4 ± 5.6 vs. 14.7 ± 5.9 mmHg, p < 0.001). ROSC was observed in six (60%) animals treated with 3:1 compression to ventilation ratio and nine (90%) animals treated with continuous chest compressions and asynchronous ventilation (p = 0.30). Time to ROSC was significantly lower in the experimental group (30 (30-30) vs. 60 (60-60) sec, p = 0.021). Of note, 7 (77.8%) animals in the experimental group and 1 (16.7%) animal in the control group achieved ROSC after 30 s (0.02). At 4 h, 2 (20%) animals survived in the control group compared to 7 (70%) animals in the experimental group (p = 0.022).
Conclusion : Continuous chest compressions with asynchronous ventilations significantly improved CPP, ETCO2, time to ROSC, ROSC at 30 s and survival in a porcine model of neonatal resuscitation.
Conclusion (proposition de traduction) : Les compressions thoraciques continues associées à une ventilation asynchrone ont significativement amélioré la perfusion coronaire, l'ETCO2, le temps jusqu'au RACS, le RACS à 30 s et la survie dans un modèle porcin de réanimation néonatale.
Commentaire : RACS : retour à une activité circulatoire (ou cardiaque) spontanée
Clinical predictors of delayed neurological sequelae in charcoal-burning carbon monoxide poisoning.
Sert ET, Kokulu K, Mutlu H. | Am J Emerg Med. 2021 Oct;48:12-17
DOI: https://doi.org/10.1016/j.ajem.2021.04.001
Keywords: Carbon monoxide; Charcoal; Delayed neurological sequelae; Neurotoxicity; Poisoning.
Research article
Introduction : The main objective of the treatment of acute carbon monoxide (CO) poisoning is to prevent delayed neurological sequelae (DNS). However, today there is still no objective screening tool to identify patients at high risk of developing DNS. The aim of this study was to identify clinical factors that could predict DNS after acute charcoal-burning CO poisoning.
Méthode : This prospective observational study was conducted from September 1, 2019 to August 31, 2020 in a single academic medical center. Patients older than 18 years of age suffering from charcoal-burning CO poisoning were included in the study. After acute recovery, patients were followed up for six weeks to investigate for DNS development. The clinical predictors of DNS were determined using a multivariate logistic regression model.
Résultats : Of the 217 patients-113 males (52.1%), median age 37.0 (27.5-51.5) years-included, 49 (22.6%) developed DNS. The multivariate logistic regression analysis revealed the independent predictors of DNS as a lower initial Glasgow Coma Scale (GCS) score (adjusted odds ratio (AOR): 0.73, 95% confidence interval (CI): 0.62-0.87), a longer duration of CO exposure (AOR: 2.18, 95% CI: 1.65-2.88), and the presence of acute brain lesions with high signal intensity on diffusion-weighted imaging (AOR: 5.22, 95% CI: 1.50-18.08). The created multivariate regression model predicted DNS development with high accuracy (area under the curve: 0.93, 95% CI: 0.89-0.97).
Conclusion : A low initial GCS score, longer exposure to CO and abnormal findings on diffusion-weighted magnetic resonance imaging can assist in the early identification of patients at high risk of DNS development.
Conclusion (proposition de traduction) : Un score initial de Glasgow faible, une exposition plus longue au CO et des résultats anormaux sur l'imagerie par résonance magnétique pondérée en diffusion peuvent aider à l'identification précoce des patients à haut risque de développement retardé de séquelles neurologiques.
Commentaire : Le syndrome post-intervallaire, dont la prévalence varie de 1 à 40 %, est une complication de l'intoxication au CO caractérisée par une symptomatologie neuropsychiatrique, de gravité variable, et d'apparition potentiellement retardée après un intervalle libre de 3 semaines.
Comparison of qSOFA, SIRS, and NEWS scoring systems for diagnosis, mortality, and morbidity of sepsis in emergency department.
Oduncu AF, Kıyan GS, Yalçınlı S. | Am J Emerg Med. 2021 Oct;48:54-59
DOI: https://doi.org/10.1016/j.ajem.2021.04.006
Keywords: Emergency room; Mortality; NEWS; SIRS; Sepsis; qSOFA.
Research article
Introduction : This study was aimed to compare the quick Sequential Organ Failure Assessment (qSOFA), Systemic Inflammatory Response Syndrome (SIRS), and National Early Warning Score (NEWS) scoring systems for diagnosing sepsis and predicting mortality and morbidity.
Méthode : A prospective study was designed. qSOFA, SIRS, and NEWS scores were calculated at the admission. The diagnosis of sepsis was made with SOFA scoring initially. The morbidity and mortality of the patients were identified during follow-up. Also, the sensitivity, specificity, negative predictive value, and positive predictive value of three scoring systems were calculated. The scoring systems were compared with ROC analysis.
Résultats : A total of 463 patients were evaluated. There were 287 (62.0%) patients diagnosed with sepsis, and septic shock occurred in 64 (13.8%) of patients. Seven-day mortality rate was 8.4% (n = 39), 30-day mortality rate was 18.1% (n = 84). The sensitivity for qSOFA, SIRS, and NEWS for diagnosis of sepsis was 23%, 77%, 58%, and specificity was 99%, 35%, 81% respectively. The sensitivity of the qSOFA, SIRS and NEWS scoring systems for mortality was 39%, 82%, 77% and specificity 91%, 29%, and 64%, respectively. AUROC values for mortality detected as NEWS = 0.772, qSOFA = 0.758, SIRS = 0.542. According to the ROC analysis, the SIRS system was significantly less useful than the qSOFA and NEWS system in the diagnosis of sepsis and mortality (p < 0.0001).
Conclusion : NEWS and qSOFA scoring systems have similar prognosis in both diagnosing sepsis and predicting mortality and both are superior to SIRS.
Conclusion (proposition de traduction) : Les scores NEWS et qSOFA ont un pronostic similaire pour le diagnostic du sepsis et la prédiction de la mortalité et les deux sont supérieurs au SIRS.
The role of the BUN/albumin ratio in predicting mortality in COVID-19 patients in the emergency department.
Küçükceran K, Ayrancı MK, Girişgin AS, Koçak S, Dündar ZD. | Am J Emerg Med. 2021 Oct;48:33-37
DOI: https://doi.org/10.1016/j.ajem.2021.03.090
| Télécharger l'article au format
Keywords: Blood Urea Nitrogen; COVID-19; In-hospital mortality; Serum Albumin.
Research article
Introduction : Due to the high mortality and spread rates of coronavirus disease 2019 (COVID-19), there are currently serious challenges in emergency department management. As such, we investigated whether the blood urea nitrogen (BUN)/albumin ratio (BAR) predicts mortality in the COVID-19 patients in the emergency department.
Méthode : A total of 602 COVID-19 patients who were brought to the emergency department within the period from March to September 2020 were included in the study. The BUN level, albumin level, BAR, age, gender, and in-hospital mortality status of the patients were recorded. The patients were grouped by in-hospital mortality. Statistical comparison was conducted between the groups.
Résultats : Of the patients who were included in the study, 312(51.8%) were male, and their median age was 63 years (49-73). There was in-hospital mortality in 96(15.9%) patients. The median BUN and BAR values of the patients in the non-survivor group were significantly higher than those in the survivor group (BUN: 24.76 [17.38-38.31] and 14.43 [10.84-20.42], respectively [p < 0.001]; BAR: 6.7 [4.7-10.1] and 3.4 [2.5-5.2], respectively [p < 0.001]). The mean albumin value in the non-survivor group was significantly lower than that in the survivor group (3.60 ± 0.58 and 4.13 ± 0.51, respectively; p < 0.001). The area-under-the-curve (AUC) and odds ratio values obtained by BAR to predict in-hospital COVID-19 mortality were higher than the values obtained by BUN and albumin (AUC of BAR, BUN, and albumin: 0.809, 0.771, and 0.765, respectively; odds ratio of BAR>3.9, BUN>16.05, and albumin<4.01: 10.448, 7.048, and 6.482, respectively).
Conclusion : The BUN, albumin, and BAR levels were found to be reliable predictors of in-hospital mortality in COVID-19 patients, but BAR was found to be a more reliable predictor than the BUN and albumin levels.
Conclusion (proposition de traduction) : Les taux d'urée, d'albumine et le rapport urémie/albumine se sont avérés être des prédicteurs fiables de la mortalité hospitalière chez les patients COVID-19, mais le rapport urémie/albumine s'est avéré être un prédicteur plus fiable que les taux d'urémie et d'albumine.
How does the side of approach impact the force delivered during external chest compression?.
Tsou JY, Kao CL, Hong MY, Chang CJ, Su FC, Chi CH. | Am J Emerg Med. 2021 Oct;48:67-72
DOI: https://doi.org/10.1016/j.ajem.2021.03.085
Keywords: Biomechanical; Cardiopulmonary resuscitation; External chest compression; Manikin; Pressure measuring system.
Research articl
Introduction : We investigated the biomechanics of four external chest compression (ECC) approaches involving different sides of approach and hand placement during cardiopulmonary resuscitation (CPR).
Méthode : A total of 60 participants (30 women and 30 men) with CPR certification performed standard continuous 2-min ECC on a Resusci Anne manikin with real-time feedback in four scenarios: rescuer at the manikin's right side with right hand chest contact (RsRc), rescuer at the manikin's right side with left hand chest contact (RsLc), rescuer at the manikin's left side with left hand chest contact (LsLc), and rescuer at the manikin's left side with right hand chest contact (LsRc). Pressure distribution maps of the palm, peak compression pressure, and compression forces were analysed.
Résultats : The participants' mean age, height, and weight was 24.8 ± 4.8 years, 165.8 ± 8.7 cm, and 62.7 ± 13.5 kg, respectively. Of the participants, 58 and 2 were right- and left-handed, respectively. Significant between-scenario differences were observed in ulnar-side palm pressure. Ulnar-radial pressure differences were higher in the LsLc and RsRc groups than in the LsRc and RsLc groups (0.69 ± 0.62 and 0.73 ± 050 kg/cm2 vs. 0.49 ± 0.49 and 0.50 ± 0.59 kg/cm2; respectively; p < 0.05). Ulnar-radial force differences were higher in the LsLc and RsRs groups than in the sLsLc and RsRs groups.
Conclusion : The higher differences in pressure and force under the LsLc and RsRc approaches may lead to higher risks of potential injury. When performing standard-quality ECC, the LsRc and RsLc approaches, in which compression pressure and force are better distributed, may be more suitable than RsRc or LsLc.
Conclusion (proposition de traduction) : Les différences plus importantes de pression et de force sous le côté gauche avec contact thoracique avec la main gauche et le côté droit avec contact thoracique avec la main droite peuvent entraîner des risques de blessures plus élevés. Lors d’une compression thoracique externe de qualité standard, le côté gauche avec contact thoracique droit et le côté droit avec contact thoracique gauche approches, dans lequel la pression et la force de compression sont mieux répartis, peut être plus approprié que le côté droit avec contact avec la poitrine de la main droite ou le côté gauche avec contact avec la poitrine de la main gauche.
Diltiazem versus metoprolol for the management of atrial fibrillation: A systematic review and meta-analysis.
Jafri SH, Xu J, Warsi I, Cerecedo-Lopez CD. | Am J Emerg Med. 2021 Oct;48:323-327
DOI: https://doi.org/10.1016/j.ajem.2021.06.053
Keywords: Aucun
Research article
Editorial : Atrial fibrillation (AF) is the most common pathological cardiac arrhythmia, affecting more than 33 million people around the globe. AF is broadly classified based on the duration of cardiac arrhythmia; pAF lasting less than one-week (paroxysmal AF), duration between one-week to one-year (persistenet AF), and duration greater than one-year (long-standing, persistent AF). Regardless of classification, the management of AF aims at three main objectives: etiological diagnosis, complication prevention, and heart rate (HR) control. Treatment of pAF can be classified into rate- and rhythm-control strategies. Both can improve symptoms, but neither has been conclusively shown to improve survival compared with other, with the exception of high-cardiovascular-risk patientswho are treated early in the course of their disease, as it was recently shown in EAST AFNET4 trial. Rate control startegy addresses symptoms related to pAF, it is commonly the first step in the management of patients with pAF and other supraventricular tachycardias. Agents used for rate control include non-dihydropyridine calcium channel blockers and non-selective beta-blockers. Both types of agents target the atrioventricular node of the cardiac electrical conduction systemto hinder the reverberant electrical impulses created in the atrial cardiac tissue during AF. The most common non-dihydropyridine calcium channel blocker and non-selective beta-blocker used in the management of pAF are diltiazem and metoprolol, respectively, with both agents being used interchangeably according to physician preference, patient characteristics and availability. Specific recommendations on the use of one agent vs. the other have not been formally advanced. Recently, few retrospective studies and a small number of trials have compared the use of diltiazem vs. metoprolol for the management of pAF.
Conclusion : Our analysis did demonstrate a faster HR normalization with diltiazem that could be considered “significant” in traditional terminology. In addition, our analysis revealed larger differences in HR in the immediate periods after the administration of diltiazem. When pooled together, these findings suggest that diltiazem may be more effective in achieving HR control rapidly in patients with pAF.
In terms of safety, no differences in SBPwere identified between the diltiazem and metoprolol group of studies evaluating these drugs for the management of pAF. Given the lack of data availability from the Frommet al. study, Martindale et al. were not able to assess differences in BP between the groups.
Conclusion (proposition de traduction) : Notre analyse a démontré une normalisation de la fréquence cardiaque plus rapide avec le diltiazem qui pourrait être considérée comme « importante » dans la terminologie traditionnelle. De plus, notre analyse a révélé des différences plus importantes de fréquence cardiaque dans les périodes immédiates après l'administration de diltiazem. Combinés, ces résultats suggèrent que le diltiazem peut être plus efficace pour contrôler rapidement la fréquence cardiaque chez les patients présentant une fibrillation atriale paroxystique.
En termes de sécurité, aucune différence avec la pression artérielle systolique n'a été identifiée entre le diltiazem et le groupe d'études métoprolol évaluant ces médicaments pour la gestion de la fibrillation atriale paroxystique. Étant donné le manque de disponibilité des données de Frommet al. étude, Martindale et al. n'ont pas été en mesure d'évaluer les différences de pression artérielle entre les groupes.
The British Medical Journal
Cardioversion in patients with newly diagnosed non-valvular atrial fibrillation: observational study using prospectively collected registry data.
Pope MK, Hall TS, Schirripa V, Radic P, Virdone S, Pieper KS, Le Heuzey JY, Jansky P, Fitzmaurice DA, Cappato R, Atar D, Camm AJ, Kakkar AK; GARFIELD-AF investigators. | BMJ. 2021 Oct 27;375:e066450
DOI: https://doi.org/10.1136/bmj-2021-066450
| Télécharger l'article au format
Keywords: Aucun
Research
Introduction : To investigate the clinical outcomes of patients who underwent cardioversion compared with those who did not have cardioverson in a large dataset of patients with recent onset non-valvular atrial fibrillation.
Design: Observational study using prospectively collected registry data (Global Anticoagulant Registry in the FIELD-AF-GARFIELD-AF).
Méthode : 1317 participating sites in 35 countries.
Participants: 52 057 patients aged 18 years and older with newly diagnosed atrial fibrillation (up to six weeks' duration) and at least one investigator determined stroke risk factor.
Main outcome measures: Comparisons were made between patients who received cardioversion and those who had no cardioversion at baseline, and between patients who received direct current cardioversion and those who had pharmacological cardioversion. Overlap propensity weighting with Cox proportional hazards models was used to evaluate the effect of cardioversion on clinical endpoints (all cause mortality, non-haemorrhagic stroke or systemic embolism, and major bleeding), adjusting for baseline risk and patient selection.
Résultats : 44 201 patients were included in the analysis comparing cardioversion and no cardioversion, and of these, 6595 (14.9%) underwent cardioversion at baseline. The propensity score weighted hazard ratio for all cause mortality in the cardioversion group was 0.74 (95% confidence interval 0.63 to 0.86) from baseline to one year follow-up and 0.77 (0.64 to 0.93) from one year to two year follow-up. Of the 6595 patients who had cardioversion at baseline, 299 had a follow-up cardioversion more than 48 days after enrolment. 7175 patients were assessed in the analysis comparing type of cardioversion: 2427 (33.8%) received pharmacological cardioversion and 4748 (66.2%) had direct current cardioversion. During one year follow-up, event rates (per 100 patient years) for all cause mortality in patients who received direct current and pharmacological cardioversion were 1.36 (1.13 to 1.64) and 1.70 (1.35 to 2.14), respectively.
Conclusion : In this large dataset of patients with recent onset non-valvular atrial fibrillation, a small proportion were treated with cardioversion. Direct current cardioversion was performed twice as often as pharmacological cardioversion, and there appeared to be no major difference in outcome events for these two cardioversion modalities. For the overall cardioversion group, after adjustments for confounders, a significantly lower risk of mortality was found in patients who received early cardioversion compared with those who did not receive early cardioversion.
Conclusion (proposition de traduction) : Dans ce vaste ensemble collectif de patients présentant une fibrillation atriale non valvulaire de découverte récente, une petite proportion a été traitée par cardioversion. La cardioversion à courant continu a été réalisée deux fois plus souvent que la cardioversion pharmacologique, et il ne semblait pas y avoir de différence majeure dans les événements de résultat pour ces deux modalités de cardioversion. Pour l'ensemble du groupe de cardioversion, après ajustements pour les facteurs de confusion, un risque de mortalité significativement plus faible a été trouvé chez les patients qui ont bénéficié d'une cardioversion précoce par rapport à ceux qui n'ont pas bénéficié de cardioversion précoce.
The Journal of Emergency Medicine
Admission Blood Glucose in the Emergency Department is Associated with Increased In-Hospital Mortality in Nontraumatic Critically Ill Patients.
Bernhard M, Kramer A, Döll S, Weidhase L, Hartwig T, Petros S, Gries A. | J Emerg Med. 2021 Oct;61(4):355-364
DOI: https://doi.org/10.1016/j.jemermed.2021.04.011
Keywords: Admission glucose; Emergency department; Mortality; Nontraumatic critically ill; Resuscitation room.
Original Contribution
Introduction : Abnormal admission blood glucose was reported as a useful predictor of outcome in critically ill patients.
Objectives: To identify patients at higher risk, this study aimed to evaluate the relationship between admission blood glucose levels and patient mortality during the management of nontraumatic critically ill patients in the emergency department (ED).
Méthode : In this prospective, single-center observational study in a German university ED, all adult patients admitted to the resuscitation room of the ED were included between September 1, 2014 and August 31, 2015. Directly after resuscitation room admission, blood samples for admission blood glucose were taken, and adult patients were divided into groups according to predefined cut-offs between the admission blood glucose. Study endpoint was in-hospital mortality.
Résultats : During the study period, 532 patients were admitted to the resuscitation room. The data of 523 patients (98.3%) were available for analysis. The overall in-hospital mortality was 34.2%. In comparison with an in-hospital mortality of 25.2% at an admission blood glucose of 101-136 mg/dL (n = 107), admission blood glucose of ≤ 100 mg/dL (n = 25, odds ratio [OR] 6.30, 95% confidence interval [CI] 2.44-16.23, p < 0.001), 272-361 mg/dL (n = 63, OR 2.53, 95% CI 1.31-4.90, p = 0.007), and ≥ 362 mg/dL (n = 44, OR 2.96, 95% CI 1.42-6.18, p = 0.004) were associated with a higher mortality.
Conclusion : Abnormal admission blood glucose is associated with a high in-hospital mortality. Admission blood glucose is an inexpensive and rapidly available laboratory parameter that may predict mortality and help to identify critically ill patients at risk in a general nontraumatic critically ill ED patient cohort. The breakpoint for in-hospital mortality may be an admission blood glucose ≤ 100 and ≥ 272 mg/dL.
Conclusion (proposition de traduction) : Une glycémie anormale à l'admission est associée à une mortalité élevée à l'hôpital. La glycémie à l'admission est un paramètre de laboratoire peu coûteux et rapidement disponible qui peut prédire la mortalité et aider à identifier les patients gravement malades à risque dans une cohorte générale de patients gravement malades aux urgences non traumatiques.
Le seuil de mortalité à l'hôpital peut être une glycémie à l'admission ≤ 100 et ≥ 272 mg/dL (ndlr : ≤ 5,6 mol/L et ≥ 15,1 mmol/L).
Diagnosis and Management of the Critically Ill Adult Patient with Hyperglycemic Hyperosmolar State.
Long B, Willis GC, Lentz S, Koyfman A, Gottlieb M. | J Emerg Med. 2021 Oct;61(4):365-375
DOI: https://doi.org/10.1016/j.jemermed.2021.05.008
Keywords: diabetes; endocrine; hyperglycemia; hyperglycemic hyperosmolar state; hyperosmolar; hyperosmotic hyperglycemic nonketotic state.
Clinical Review
Introduction : Hyperglycemic hyperosmolar state is a life-threatening complication of diabetes mellitus. Therefore, it is important for emergency physicians to be aware of this unique diagnosis and treatment considerations.
Méthode : This manuscript reviews the emergency department evaluation and management of the adult patient with hyperglycemic hyperosmolar state.
Discussion : Hyperglycemic hyperosmolar state is diagnosed by an elevated glucose, elevated serum osmolality, minimal or absent ketones, and a neurologic abnormality, most commonly altered mental status. Treatment involves fluid resuscitation and correction of electrolyte abnormalities. It is important to monitor these patients closely to avoid overcorrection of osmolality, sodium, and other electrolytes. These patients are critically ill and generally require admission to an intensive care unit.
Conclusion : Hyperglycemic hyperosmolar state is associated with significant morbidity and mortality. It is important for clinicians to be aware of the current evidence regarding the diagnosis, management, and disposition of these patients.
Conclusion (proposition de traduction) : Le coma hyperosmolaire est associé à une morbidité et une mortalité importantes. Il est important que les cliniciens soient au courant des données probantes actuelles concernant le diagnostic, la prise en charge et le traitement de ces patients.
Commentaire : Le coma hyperosmolaire devrait être appelé syndrome d'hyperosmolarité hyperglycémique (SHH).
Coma hyperosmolaire .
Battlefield Acupuncture Versus Standard Pharmacologic Treatment of Low Back Pain in the Emergency Department: A Randomized Controlled Trial.
Johnston K, Bonjour T, Powell J, April MD. | J Emerg Med. 2021 Oct;61(4):406-415
DOI: https://doi.org/10.1016/j.jemermed.2021.07.017
Keywords: acupuncture; analgesia; battlefield acupuncture; emergency department; pain.
Brief Report
Introduction : Battlefield acupuncture (BFA) offers a novel analgesic option that avoids the need for pharmacologic interventions with problematic side effect profiles.
titre_en_plusx: To compare BFA with standard pharmacologic interventions to treat patients in the emergency department (ED) with low back pain.
Méthode : We conducted a nonblinded randomized controlled trial of a convenience sample of adults presenting to an urban tertiary care ED with a chief complaint of low back pain. We randomized subjects to undergo either BFA or the control arm in which they received standard pharmacologic therapies at the discretion of their treating clinician. The primary outcome was mean pain reduction measured on a 100-mm visual analogue scale (VAS) from enrollment to 30-40 min postintervention. Secondary outcomes included the Back Pain Functional Scale (BPFS; scores range from 0-60) measured at 30-40 min postintervention and again at 48-72 h postintervention.
Résultats : We enrolled 52 subjects with 26 randomized to each arm. The mean decrease in pain VAS was 33.4 mm among patients undergoing BFA vs. 21.5 mm in the control arm (effect size difference 12.0 mm [95% confidence interval {CI} 0.1-23.8 mm]). The median improvement in the BPFS score at 48-72 h postintervention was 12.0 among patients undergoing BFA vs. 8.0 in the control arm (effect size difference 4 [95% CI -9.0 to 16.0]). There were no adverse events.
Conclusion : BFA shows promise for further study as an alternative to standard pharmacologic interventions among adults presenting to the ED with low back pain.
Conclusion (proposition de traduction) : L'auriculothérapie est prometteuse pour une étude plus approfondie en tant qu'alternative aux interventions pharmacologiques standard chez les adultes se présentant aux urgences pour une lombalgie.
The Journal of Trauma and Acute Care Surgery
Prehospital shock index and systolic blood pressure are highly specific for pediatric massive transfusion.
Zhu CS, Braverman M, Goddard S, McGinity AC, Pokorny D, Cotner-Pouncy T, Eastridge BJ, Epley S, Greebon LJ, Jonas RB, Liao L, Nicholson SE, Schaefer R, Stewart RM, Winckler CJ, Jenkins DH. | J Trauma Acute Care Surg. 2021 Oct 1;91(4):579-583
DOI: https://doi.org/10.1097/ta.0000000000003275
Keywords: Aucun
PTS 2020 PODIUM
Introduction : While massive transfusion protocols (MTPs) are associated with decreased mortality in adult trauma patients, there is limited research on the impact of MTP on pediatric trauma patients. The purpose of this study was to compare pediatric trauma patients requiring massive transfusion with all other pediatric trauma patients to identify triggers for MTP activation in injured children.
Méthode : Using our level I trauma center's registry, we retrospectively identified all pediatric trauma patients from January 2015 to January 2018. Massive transfusion (MT) was defined as infusion of 40 mL/kg of blood products in the first 24 hours of admission. Patients missing prehospital vital sign data were excluded from the study. We retrospectively collected data including demographics, blood utilization, variable outcome data, prehospital vital signs, prehospital transport times, and Injury Severity Scores. Statistical significance was determined using Mann-Whitney U test and χ2 test. p Values of less than 0.05 were considered significant.
Résultats : Thirty-nine (1.9%) of the 2,035 pediatric patients met the criteria for MT. All-cause mortality in MT patients was 49% (19 of 39 patients) versus 0.01% (20 of 1996 patients) in non-MT patients. The two groups significantly differed in Injury Severity Score, prehospital vital signs, and outcome data.Both systolic blood pressure (SBP) of <100 mm Hg and shock index (SI) of >1.4 were found to be highly specific for MT with specificities of 86% and 92%, respectively. The combination of SBP of <100 mm Hg and SI of >1.4 had a specificity of 94%. The positive and negative predictive values of SBP of <100 mm Hg and SI of >1.4 in predicting MT were 18% and 98%, respectively. Based on positive likelihood ratios, patients with both SBP of <100 mm Hg and SI of >1.4 were 7.2 times more likely to require MT than patients who did not meet both of these vital sign criteria.
Conclusion : Pediatric trauma patients requiring early blood transfusion present with lower blood pressures and higher heart rates, as well as higher SIs and lower pulse pressures. We found that SI and SBP are highly specific tools with promising likelihood ratios that could be used to identify patients requiring early transfusion.
Conclusion (proposition de traduction) : Les patients traumatisés pédiatriques nécessitant une transfusion sanguine précoce présentent des pressions artérielles plus basses et des fréquences cardiaques plus élevées, ainsi que des « Shock Index » plus élevés et des pressions artérielles plus basses. Nous avons constaté que le « Shock Index » et la pression artérielle systolique sont des outils très spécifiques avec des rapports de probabilité prometteurs qui pourraient être utilisés pour identifier les patients nécessitant une transfusion précoce.
The Lancet
Cardiopulmonary resuscitation in special circumstances.
Soar J, Becker LB, Berg KM, Einav S, Ma Q, Olasveengen TM, Paal P, Parr MJA. | Lancet. 2021 Oct 2;398(10307):1257-1268
DOI: https://doi.org/10.1016/s0140-6736(21)01257-5
Keywords: Aucun
SERIES - Cardiac Arrest
Editorial : Cardiopulmonary resuscitation prioritises treatment for cardiac arrests from a primary cardiac cause, which make up the majority of treated cardiac arrests. Early chest compressions and, when indicated, a defibrillation shock from a bystander give the best chance of survival with a good neurological status. Cardiac arrest can also be caused by special circumstances, such as asphyxia, trauma, pulmonary embolism, accidental hypothermia, anaphylaxis, or COVID-19, and during pregnancy or perioperatively. Cardiac arrests in these circumstances represent an increasing proportion of all treated cardiac arrests, often have a preventable cause, and require additional interventions to correct a reversible cause during resuscitation. The evidence for treating these conditions is mostly of low or very low certainty and further studies are needed. Irrespective of the cause, treatments for cardiac arrest are time sensitive and most effective when given early-every minute counts.
Conclusion : Cardiac arrest in special circumstances, such as asphyxia, trauma, pulmonary embolism, accidental hypothermia, anaphylaxis, COVID-19, during pregnancy, or periopera- tively, are an increasing proportion of all treated cardiac arrests. Cardiac arrest is often preventable, but when cardiac arrest occurs, patients require additional early interventions to correct a reversible cause during resuscitation.
Conclusion (proposition de traduction) : Les arrêts cardiaques dans des circonstances particulières, comme l'asphyxie, les arrêts traumatiques, l'embolie pulmonaire, l'hypothermie accidentelle, l'anaphylaxie, la COVID-19, pendant la grossesse ou en périopératoire, représentent une proportion croissante de tous les arrêts cardiaques traités. L'arrêt cardiaque est souvent évitable, mais lorsqu'un arrêt cardiaque survient, les patients nécessitent des interventions précoces supplémentaires pour corriger une cause réversible pendant la réanimation.
The New England Journal of Medicine
Point-of-Care Ultrasonography.
Díaz-Gómez JL, Mayo PH, Koenig SJ. | N Engl J Med. 2021 Oct 21;385(17):1593-1602
DOI: https://doi.org/10.1056/nejmra1916062
Keywords: Aucun
REVIEW ARTICLE
Editorial : Point-of-care ultrasonography (POCUS) is defined as the acquisition, interpretation, and immediate clinical integration of ultrasonographic imaging performed by a treating clinician at the patient’s bedside rather than by a radiologist or cardiologist. POCUS is an inclusive term; it is not limited to any specialty, protocol, or organ system. With the advent of smaller and more affordable ultrasound machines, combined with evidence that nonradiologists and noncardiologists can become competent in the performance of POCUS, it is now used in many practice settings and in all phases of care — from screening and diagnosis to procedural guidance and monitoring — and has become associated with changes in clinical decision making in medical practice. A recent study showed that POCUS facilitated confirmation of the suspected clinical diagnosis in up to 50% of cases and supported a change in the initial diagnosis in 23% of cases. In this review, we discuss key trends in POCUS technology, advances in its clinical applications, and the overlap and complementarity of POCUS and consultative ultrasonography in primary imaging specialties.
Conclusion : The use of POCUS is not limited to one specialty, protocol, or organ system. POCUS provides the treating clinician with real-time diagnostic and monitoring information and can be used to enhance the safety of standard ultrasound-guided procedures. The introduction of POCUS curricula and training at the medical school and postgraduate levels, the increasing level of evidence of its effect in clinical practice, and advances in handheld systems all point toward the possibility that POCUS will become a standard tool of the frontline clinician. However, it will be critical to determine which, if any, applications ultimately benefit patient care.
Conclusion (proposition de traduction) : L'utilisation de l'échographie au point d'intervention n'est pas limitée à une spécialité, un protocole ou un système d'organes. L'échographie au point d'intervention fournit au clinicien traitant des informations de diagnostic et de surveillance en temps réel et peut être utilisé pour améliorer la sécurité des procédures standard guidées par échographie. L'introduction des programmes d'études et de la formation à l'échographie au point d'intervention aux niveaux de la faculté de médecine et du troisième cycle, le niveau croissant de preuves de son effet dans la pratique clinique et les progrès des systèmes portables indiquent tous la possibilité que l'échographie au point d'intervention devienne un outil standard du clinicien de première ligne. Cependant, il sera essentiel de déterminer quelles applications, le cas échéant, bénéficieront en fin de compte aux soins des patients.